First-line Ablation Reduces AF Progression, Boosts Quality of Life
The study shows “we should be thinking about ablation earlier in that management paradigm,” Jason Andrade says.

CHICAGO, IL—In a population of patients with paroxysmal atrial fibrillation (AF) deemed to be at low risk of progression, first-line cryoballoon ablation reduced the likelihood of developing persistent AF through 3 years of follow-up and was associated with a variety of other clinical benefits in the PROGRESSIVE-AF study.
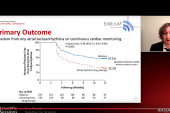
The rate of progression to persistent AF was 1.9% in patients first treated with ablation and 7.4% in those who initially received antiarrhythmic drugs (HR 0.25; 95% CI 0.09-0.70), Jason Andrade, MD (University of British Columbia, Vancouver, Canada), reported here at the American Heart Association 2022 Scientific Sessions.
An ablation-first strategy also lowered the risk of any recurrent atrial tachyarrhythmia, reduced AF burden, improved both quality of life and symptom burden, and lowered the rate of hospitalization. Overall adverse events were less frequent in the ablation arm of the study, which is the 3-year follow-up of the patients randomized in the EARLY-AF trial.
What the extended follow-up, published simultaneously online in the New England Journal of Medicine, shows is that treating patients with ablation first has a sustained, positive impact on AF progression, Andrade told TCTMD. That’s important “because once you go to persistent A-fib, the rates of stroke go up by 30%, death goes up, and heart failure hospitalization or new-onset heart failure goes up.”
Conceptually, he added, “ablation should be disease-modifying and prevent that progression, but I would say that we didn’t know that until now.”
PROGRESSIVE-AF
The EARLY-AF trial included 303 patients (mean age 58 years; 71% men) with untreated, symptomatic, paroxysmal AF randomized to first-line cryoballoon ablation or antiarrhythmic drugs (AADs). The population was relatively young and healthy, but their AF was severely impairing health-related quality of life. As previously reported, the risk of AF recurrence at 1 year as measured using implantable loop recorders was lower in the ablation group.
PROGRESSIVE-AF is the phase of the study extending follow-up out to 3 years to enable a look at progression of disease. In theory, ablation will modify the pathogenic mechanism of AF, limit disease progression, and ultimately improve clinical outcomes, Andrade said.
In this study, persistent AF was defined as AF, atrial flutter, or atrial tachycardia lasting at least 7 days or lasting 2 to 7 days and requiring cardioversion for termination. By 3 years, significantly fewer patients had progressed to persistent AF in the ablation arm versus the AAD arm, a result that was consistent regardless of which definition of persistent AF was used.
Among secondary outcomes, the risk of any recurrent atrial tachyarrhythmia lasting at least 30 seconds was lower in the ablation arm (56.5% vs 77.2%; HR 0.51; 95% CI 0.38-0.67). AF burden was lower, too.
Patient-reported outcomes, including disease-specific and general quality of life and symptom burden, also significantly favored an ablation-first strategy. First-line ablation was associated with lower risks of hospitalization (5.2% vs 16.8%; RR 0.31; 95% CI 0.14-0.66) and non-protocol ablations (17.5% vs 42.3%; RR 0.41; 95% CI 0.28-0.61) during the 3-year follow-up period.
Overall adverse events were less frequent in the ablation arm (11.0% vs 23.5%; RR 0.47; 95% CI 0.28-0.79), although the difference in serious events didn’t reach significance (4.5% vs 10.1%; RR 0.45; 95% CI 0.19-1.05).
Changing the Doctor-Patient Discussion
Commenting for TCTMD, Luigi Di Biase, MD, PhD (Albert Einstein College of Medicine at Montefiore Hospital, Bronx, NY), noted that prior research has all pointed in the same direction—that AF will progress unless it is blocked. Prior trials have shown that first-line ablation, with either a cryoballoon or radiofrequency catheter, provides good outcomes, and the EAST-AFNET 4 trial has shown the early rhythm control is better than rate control for preventing CV events, he said.
One previous trial, ATTEST, showed that radiofrequency ablation reduces progression from paroxysmal to persistent AF among patients who had failed AAD therapy, and now PROGRESSIVE-AF expands that finding to first-line ablation in a larger patient cohort, said Di Biase, a member of the American College of Cardiology’s Electrophysiology Council.
A strength of PROGRESSIVE-AF, he added, is that it included relatively young, healthy patients who would be expected to have slow progression to persistent AF. He said that even in that group, the message is now clear: “When you have A-fib, intervene early and intervene early with ablation rather than medication.”
When you have A-fib, intervene early and intervene early with ablation rather than medication. Luigi Di Biase
Di Biase anticipated that future iterations of the guidelines will incorporate these findings to propose at least including this information in risk-benefit discussions. “Clearly this trial will force us to discuss with the patient that with medication there is a higher risk of your A-fib progressing to more episodes and this may affect overall cardiovascular outcomes,” he said.
This trial was underpowered to examine effects on hard clinical outcomes, Andrade said, but added that the few events that did occur were concentrated in the AAD arm. “Knowing what we know about progression, you’d anticipate that if you’re changing the trajectory of disease that those things will have a long-term benefit, but you’d need a much larger cohort with a much longer follow-up to see it,” he said.
Even so, with these findings, “you can make an argument that ablation should be the first treatment and drugs should be reserved for failures,” Andrade said. “And that may be a paradigm shift in how we approach new-onset A-fib, because if we can change the disease trajectory and prevent that progression and prevent those long-term outcomes, we’ll get better results from the ablation procedure, we’ll get better quality-of-life improvements and better reductions in healthcare utilization, and overall improve long-term outcomes.”
Carina Blomström-Lundqvist, MD, PhD (Uppsala University, Sweden), discussing the results after Andrade’s presentation, said PROGRESSIVE-AF was limited in how progression was defined. By defining progression as the development of persistent AF, it misses worsening disease in patients who still have paroxysmal AF. And thus, using that definition rather than AF burden may have underestimated progression, she said.
Still, the study shows that “first-line AF ablation significantly lowers AF progression versus initial antiarrhythmic drug therapy in paroxysmal AF patients” and provides meaningful improvements in quality of life, she said, noting, however, that progression occurs only in a minority of patients and the optimal patient for first-line ablation remains unclear.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Andrade JG, Deyell MW, Macle L, et al. Progression of atrial fibrillation after cryoablation or drug therapy. N Engl J Med. 2022;Epub ahead of print.
Disclosures
- The study was supported by a peer-reviewed grant from the Cardiac Arrhythmia Network of Canada, which is a Networks of Centres of Excellence program funded from a joint initiative of the Natural Sciences and Engineering Research Council, the Social Sciences and Humanities Research Council, the Canadian Institutes of Health Research, Industry Canada, and Health Canada; by unrestricted grants from Medtronic and Baylis Medical; and by in-kind support from Medtronic (implantable cardiac monitors) and the University of British Columbia.
- Andrade reports honoraria from Abbott Canada, Biosense Webster, Biotronik, and Medtronic; institutional grants/contracts from Baylis Medical, the Heart and Stroke Foundation of Canada, and Medtronic; and a grant/contract from the Michael Smith Foundation for Health Research.
- Di Biase reports being a consultant for Stereotaxis, Biosense Webster, Boston Scientific, Abbott Medical, and Rhythm Management; and having received speaker honoraria/travel support from Biotronik, Medtronic, AtriCure, Bristol Myers Squibb, and Pfizer.
- Blomström-Lundqvist reports honoraria from Medtronic, Boston Scientific, Bayer, MSD, Sanofi, and Philips.




Comments