As US Rollout Begins for Coronary DCBs, Interventionalists Mull Practice Changes
Operators predict a shift in how they’ll treat in-stent restenosis, and maybe more, in coming years.
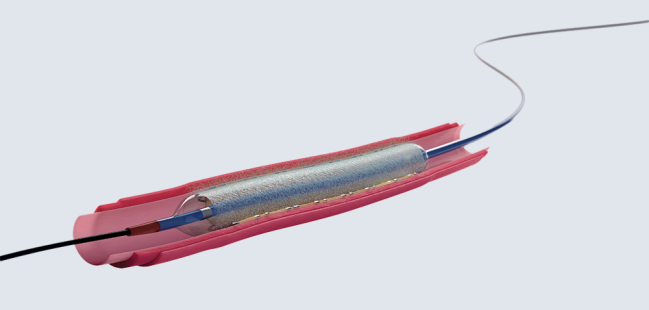
Photo Credit: Adapted from Boston Scientific
Following the US approval of the Agent paclitaxel-coated balloon for the treatment of in-stent restenosis (ISR), the first coronary procedures with the device were performed Tuesday morning at two centers in the Northeast as Boston Scientific continues its rollout.
Although drug-coated balloons (DCB) have been used for coronary procedures for several years in Europe and elsewhere, these procedures—performed at St. Francis Hospital in Roslyn, NY, and Beth Israel Deaconess Medical Center in Boston, MA—mark a milestone for US operators who have been waiting for the technology as an alternative to placing additional layers of stents or using plain old balloon angioplasty to treat ISR.
“We’re very excited to bring this technology to the US. This been something that US clinicians have been asking for,” Janar Sathananthan, MBChB, MPH, chief medical officer for interventional cardiology therapies at Boston Scientific, told TCMTD. He noted that the process of getting approval from the US Food and Drug Administration—which came at the beginning of March—“was not an easy and quick journey.”
That approval was based on the interim results of the AGENT IDE trial, which showed that patients treated with the DCB versus conventional balloon angioplasty had a lower rate of target lesion failure through 1 year, mostly driven by reduced rates of TLR and target-vessel MI. Full results released shortly after FDA approval of the device confirmed the benefits.
A new era in IC in the USA! The 1st commercial DCB @StFrancis_LI @CHS_LI in partnership with @BSCCardiology #agent. #richierich @ESHLOF @DrAllenJ @OPCILive @midwest_22 @gary62167592 @GENTILEJ1A @djc795 @JWMoses @FernanOCT @rwyeh pic.twitter.com/fCdnPuPnQA
— Ziad Ali (@ziadalinyc) April 30, 2024
Boston Scientific is currently working on getting the Agent DCB to US cath labs with a plan to “transition into a full market release over the summer,” according to another company representative.
Indeed, said Sathananthan, who is also an interventional cardiologist at St. Paul’s Hospital and Vancouver General Hospital, Canada, “this is very much going to be in people’s hands in 2024.”
Anticipating a Big Impact
Interventional cardiologists contacted by TCTMD, many of whom were still awaiting the arrival of the Agent DCB on their cath lab shelves, predicted major changes in the treatment of ISR moving forward.
Margaret McEntegart, MD, PhD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), previously worked in the United Kingdom and had access to coronary DCB for several years. “After moving to the US, I had to reset my practice to not having them available,” she said.
Based on her prior experience, the DCB were “technically very simple to use,” said McEntegart, and “in the context of ISR, they were usually a better option than a further stent layer, and a potentially good option for small-vessel disease, distal disease, and ostial side-branch disease.”
She underscored that intravascular imaging is a key component of these procedures: “If dealing with ISR, it is essential to understand if you are dealing with an underexpanded stent, neointimal hyperplasia, or neoatherosclerosis, and whether this is calcified. It's then essential to use intravascular imaging to assess whether you have adequately modified the plaque prior to using the DCB.”
Overall, McEntegart predicted, “the introduction of coronary DCB will have a significant impact on practice.”
Ron Waksman, MD (MedStar Washington Hospital Center, Washington, DC), told TCTMD via email that for ISR, “we still use brachytherapy for multilayer stents and additional DES for a single layer.” He noted that the Agent balloon was not compared against DES in the AGENT IDE trial, “so there is no data to use it over DES,” adding that plain old balloon angioplasty “is a weak competitor” and shouldn’t be used to treat ISR.
Looking ahead to the potential impact on practice, Waksman said that once DCB have been introduced for the treatment of de novo coronary lesions, “it can easily take 30% of the stent market for PCI. The future of DCB is not so much in ISR but more in de novo lesions, adopting the ‘nothing left behind’ concept.”
Reimbursement Issues
The Agent DCB is not going to be cheap, however, which may have some impact on uptake. Waksman, for instance, said, “Currently the main limitation of using the Agent balloon is the cost, $5600, [which is] not reimbursed,” adding that money will be a major factor since there are alternatives for treating ISR.
Sathananthan noted that the specific cost varies across different healthcare systems and parts of the country, with the other Boston Scientific representative saying, “The price of the Agent DCB reflects the value of this technology in addressing a significant unmet clinical need.”
The device is not currently reimbursed by the US Centers for Medicare and Medicaid Services or other major payers, but “we’re certainly working on a process that would have a pathway to reimbursement,” Sathananthan said. The pathway involves “differentiated payment plans” that include a new technology add-on payment (NTAP) or a transitional pass-through payment (TPT). Both options “we think will certainly be a big aid to help and support adoption,” he said.
Over time, however, “we anticipate that reimbursement will improve with a very specific coronary DCB coding,” Sathananthan added.
Reimbursement issues aside, Sathananthan noted that the Agent DCB “is filling a niche need for clinicians in the sense that they have simply not had this therapy available for ISRs.” He pointed out that ISR remains a common problem, accounting for about 10% of all PCIs performed.
“I think we’re going to see just uptake in use in ISRs for sure, and we hope that with better evidence generated in the United States that there’ll be broader use of this as well,” he said.
Right now, the company is rolling out the device with an eye on ensuring regional distribution across the US, accompanied by sufficient training and education, Sathananthan said. “We are very cognizant of the fact that this is a new technology to the United States. It’s a very straightforward device to use, but we have also backed up the release of the product with quite a national approach, which is a regionally designed approach with regards to education.”
The educational component, he said, includes informing clinicians about the device and the drug coating and about the importance of appropriate lesion preparation and use of intravascular imaging to guide the procedure for these ISR cases, consistent with the company’s “modern PCI” concept incorporating three components—see, prep, and treat.
“We really see imaging as the foundation as it relates to any therapy when you come to the ‘treat’ component, whether it be with a stent or a drug-coated balloon,” Sathananthan said.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioDisclosures
- Sathananthan serves as chief medical officer for interventional cardiology therapies for Boston Scientific.
- Waksman reports being the study chair of Selution ISR and Selution DE-NOVO using the sirolimus-eluting balloon for ISR and de novo lesions up to 2.75 mm.





Martin Bergmann