Challenging LAD Ostial PCI: An Innovative Technique
by
Afzalur Rahman
July 21, 2015Operator(s)
Afzalur Rahman
Affiliation
Department of Cardiology, National Institute of Cardiovascular Diseases, Dhaka, Bangladesh
Facility / Institute
National Institute of Cardiovascular Diseases, Dhaka, Bangladesh
Clinical History
The patient is a 53 year old man, smoker, dyslipidemia presented with post infarction angina and underwent coronary angiogram. He had h/o Anterior Myocardial Infarction 7 days earlier and was thrombolysed.
Angiography
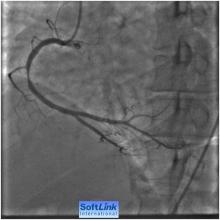
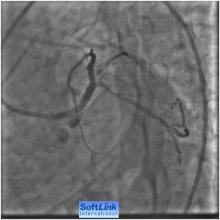
1) Normal left main coronary artery (Figure 1)
2) LAD 99% narrowing involving the LAD ostium and its proximal segment
3) LCX 30-40% at its proximal segment
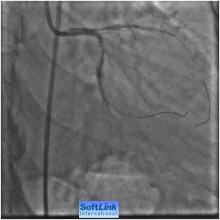
4) RCA 75-85 % at its mid segment (Figure 2)
2) LAD 99% narrowing involving the LAD ostium and its proximal segment
3) LCX 30-40% at its proximal segment
4) RCA 75-85 % at its mid segment (Figure 2)
Procedure
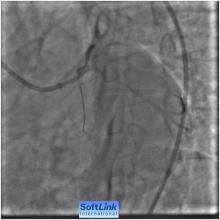
Our strategies were to perform PCI to RCA first and then LAD Ostial PCI in the same setting. For PCI to RCA: . Right Femoral route, 7F sheath was used .A 600 mg loading dose of clopidogrel 6 hours before the procedure and just before the procedure, heparin IA bolus to maintain ACT around 300 seconds. A JR 3.5, 6F guiding catheter was engaged in to RCA, 0.014 ̋ All-star wire was introduced across the lesion and then a 3.5x 18 mm BMS deployed across the lesion at 18 ATM. Post dilatation by 4.0x12 mm Quantum balloon at 14 ATM with excellent angiographic result with TIMI III flow (Figure 3).
For LAD Ostial PCI : A 7 Fr 3.5 EBU guiding catheter was engaged into LM. A 0.014" BMW guidewire (Guidant) was introduced into the distal LAD across the lesion, and another 0.014" BMW guidewire (Guidant) was introduced in to the LCX and parked there.
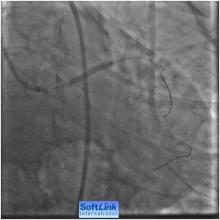
The LAD lesion was predilated by 2.0x15mm balloon at 10 atm. A 3.0 x22 mm DES (Resolute Integrity) was positioned in the LAD and then a 2.5 x15mm balloon was positioned from LM to proximal LCX and parked there. For precise LAD Ostial PCI we made sure that the proximal radio-opaque marker must be positioned proximal to the ostial LAD by super zooming, RAD caudal or LAD caudal view.
There was a balloon positioned from LM to proximal LCX. There was no oscillation of the LAD stent during positing and thus its help for precise LAD Ostial placement (Figure 4, Figure 5). Then keeping the parked balloon in position from LM to proximal LCX, the LAD stent was deployed very carefully across the lesion with precise LAD coverage at 14 atm (Figure 6). And then post dilatation by 3.5x15 mm Quantum balloon at 16 ATM. Final angiography shows excellent deployment of the stent across the lesion covering the LAD ostium adequately without any plaque shifting into LCX and without any residual narrowing and with TIMI III flow (Figure 7, Figure 8).
Post procedural course was uneventful, and the patient was discharged after 24 hours. At one year follow up, the patient remain symptom free and NYHA–I.
For LAD Ostial PCI : A 7 Fr 3.5 EBU guiding catheter was engaged into LM. A 0.014" BMW guidewire (Guidant) was introduced into the distal LAD across the lesion, and another 0.014" BMW guidewire (Guidant) was introduced in to the LCX and parked there.
The LAD lesion was predilated by 2.0x15mm balloon at 10 atm. A 3.0 x22 mm DES (Resolute Integrity) was positioned in the LAD and then a 2.5 x15mm balloon was positioned from LM to proximal LCX and parked there. For precise LAD Ostial PCI we made sure that the proximal radio-opaque marker must be positioned proximal to the ostial LAD by super zooming, RAD caudal or LAD caudal view.
There was a balloon positioned from LM to proximal LCX. There was no oscillation of the LAD stent during positing and thus its help for precise LAD Ostial placement (Figure 4, Figure 5). Then keeping the parked balloon in position from LM to proximal LCX, the LAD stent was deployed very carefully across the lesion with precise LAD coverage at 14 atm (Figure 6). And then post dilatation by 3.5x15 mm Quantum balloon at 16 ATM. Final angiography shows excellent deployment of the stent across the lesion covering the LAD ostium adequately without any plaque shifting into LCX and without any residual narrowing and with TIMI III flow (Figure 7, Figure 8).
Post procedural course was uneventful, and the patient was discharged after 24 hours. At one year follow up, the patient remain symptom free and NYHA–I.
Conclusion(s) / Result(s)
We here in report unique strategies of management of a case of PCI of challenging critical LAD ostial lesion. Our strategies were precise location of stent implantation at ostium
Simultaneous balloon placement from distal LM to proximal LCX prevented the unwanted stent movement during its placement and also properly guides us for proper precise stent placement at the ostium.
Parked balloon from distal LM to LCX will also be helpful for quick measure for any plug shifting into LCX , in case if it is occurred.
Our technique is quick, effective, and technically simple approach for successful treatment of LAD Ostial lesion. As per our knowledge this technique was not used and reported earlier.
Simultaneous balloon placement from distal LM to proximal LCX prevented the unwanted stent movement during its placement and also properly guides us for proper precise stent placement at the ostium.
Parked balloon from distal LM to LCX will also be helpful for quick measure for any plug shifting into LCX , in case if it is occurred.
Our technique is quick, effective, and technically simple approach for successful treatment of LAD Ostial lesion. As per our knowledge this technique was not used and reported earlier.
Comments/Lessons
Percutaneous intervention on LAD ostial lesions can pose unique challenges and is associated with higher procedural and medium-term complication rates. Ostial disease is traditionally defined as a lesion arising within 3 mm of the vessel origin. A decision must be made at the outset as to whether precise positioning of the stent at the ostium should be attempted, or whether stenting across the LCX back into the LMS is preferable. The presence or absence of an ostial ‘nub’ or stump to facilitate proximal positioning, The angle of the bifurcation with the LCX angles <75° are associated with greater difficulty in stent positioning and increased risk of plaque shift . The presence of significant plaque in the distal LMS or LCX ostium may dictate an alternative PCI strategy or referral for coronary artery bypass surgery. The presence of heavy calcification which may impair visualisation and stent positioning, limit stent expansion and increase the risk of stent edge dissection or restenosis.
For precise LAD Ostial PCI it is necessary to reiterate that the stent is within the radio-opaque markers on the stent balloon and thus the proximal marker must be positioned proximal to the ostial LAD.
Excessive stent movement during Stent placement may be particularly problematic with ostial LAD stenting, as seen in where oscillation of the LAD stent increases the risk of inaccurate placement.
Techniques to prevent excessive stent movement: Respiratory motion – A breath-hold, gentle shallow breathing. Cardiac motion: Pharmacological methods (such as Esmolol, Adenosine and Atropin), Rapid ventricular pacing and partial pre-inflation technique. Disadvantage: short time window may potential distress the patient can be counterproductive (Euro Intervention 2009;5:1-00). Simultaneous balloon placement is technically simple approach for prevention of unwanted stent movement during stent placement. Operators should also consider: 7 Fr guiding catheter, super zooming, RAD caudal or LAD caudal view, DES stent with High radial force and good visibility of the stent. Our technique is quick, effective, and technically simple approach for precise stent placement at LAD.
For precise LAD Ostial PCI it is necessary to reiterate that the stent is within the radio-opaque markers on the stent balloon and thus the proximal marker must be positioned proximal to the ostial LAD.
Excessive stent movement during Stent placement may be particularly problematic with ostial LAD stenting, as seen in where oscillation of the LAD stent increases the risk of inaccurate placement.
Techniques to prevent excessive stent movement: Respiratory motion – A breath-hold, gentle shallow breathing. Cardiac motion: Pharmacological methods (such as Esmolol, Adenosine and Atropin), Rapid ventricular pacing and partial pre-inflation technique. Disadvantage: short time window may potential distress the patient can be counterproductive (Euro Intervention 2009;5:1-00). Simultaneous balloon placement is technically simple approach for prevention of unwanted stent movement during stent placement. Operators should also consider: 7 Fr guiding catheter, super zooming, RAD caudal or LAD caudal view, DES stent with High radial force and good visibility of the stent. Our technique is quick, effective, and technically simple approach for precise stent placement at LAD.
Conflicts of Interest
None
We Recommend
Log in to post comments.


Rakesh Bhan
Robert Tobar