Complex PCI of Double CTO Lesion Through Left Radial Approach with High Grade Subclavian Tortuosity
by
Saidur Rahman Khan
September 4, 2012Operator(s)
Dr. Saidur Rahman Khan MD
Affiliation
Ibrahim Cardiac Hospital and Research Institute, Dhaka, Bangladesh
Facility / Institute
Ibrahim Cardiac Hospital and Research Institute, Dhaka, Bangladesh
Clinical History
A 56 year old female diabetic, hypertensive patient was admitted with the complaints of class II-III angina for the last 1 year. In the past she has always refused coronary angiography, but this time she agreed. Her ECG showed RBBB. Echocardiography revealed a normal LVEF. She was hemodynamically stable during admission and other biochemical parameters were normal. She was unwilling to do an exercise test. .
Angiography
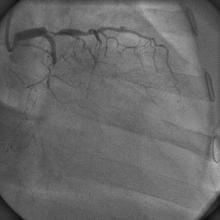
1) LAD: Totally occluded from its mid part with severe disease proximally (Figure 1)
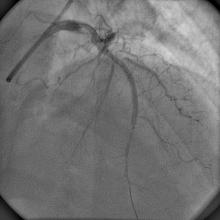
2) LCX: Totally occluded distally with feeble flow through ipsilateral collaterals (Figure 2)
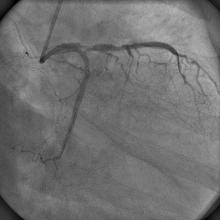
3) RCA: Mild disease in the mid RCA giving good retrograde flow to the LAD (Figure 3)
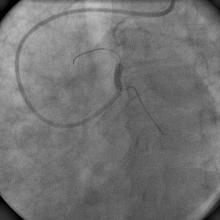
4) High grade subclavian tortuosity (Figure 4)
2) LCX: Totally occluded distally with feeble flow through ipsilateral collaterals (Figure 2)
3) RCA: Mild disease in the mid RCA giving good retrograde flow to the LAD (Figure 3)
4) High grade subclavian tortuosity (Figure 4)
Procedure
The patient was totally unwilling to go for CABG. Using a 6Fr XB3.0 guiding catheter, the LM was cannulated successfully despite the high grade tortuosity of left subclavian artery (Figure 4). A BMW guidewire was used to cross the CTO lesion of the LCX with a 2x10mm Sapphire balloon for support followed by low pressure inflation (Figure 5). TIMI II flow as established in the LCX without any flap or dissection (Figure 6) although the tip of the wire was corrugated. Keeping this guidewire in the LCX, a PT2 guidewire was used to cross the LAD lesion; and the same balloon was taken to predilate the lesion (Figure 7, Figure 8). TIMI II flow as established in the distal LAD, and a long 2.5x38mm EucaTax stent (Eucatech, Germany) was deployed in the mid LAD at 12atm (Figure 9). Before deploying the ostio-proximal LAD stent, the LCX lesion was stented using a 2.5x28mm Promus Element stent at 14atm (Figure 10). Then ostio-proximal LAD lesion was stented using an Optima stent (CID, Italy) at 18atm overlapping the distal one. (Figure 11). Distal TIMI III flow was established in both the LAD and LCX (Figure 12).
Conclusion(s) / Result(s)
The patient was hemodynamically stable during and after the procedure and was discharged after 2 days.
Comments/Lessons
It is really unpredictable to wire a CTO lesion and with high grade subclavian tortuosity. Catheter support is also not that favorable using the transradial approach. For this patient, the CTO lesions were crossed without complications or difficulties. We did not pre-plan to wire the LCX first, but stenting the LCX is reasonable before stenting the ostio-proximal LAD. Especially with this right angle origin of the LCX and LAD, crossing the ostio-proximal LAD stent to deploy a stent in the LCX may require extra effort if ostioproximal LAD is already stented.
Conflicts of Interest
None








Comments