How Should I Treat a Transient STEMI Caused by a Very Late Massive Stent Thrombosis in an Ectatic RCA?
by
Fadil Ademaj
July 1, 2013Affiliation
Medizinische Klinik- Kardiologie, Pulmologie, internistische Intensivmedizin, Eppenreutherstrasse 9, 95032 Hof, Germany
Facility / Institute
Sana Klinikum Hof
Clinical History
A 68-year-old woman was admitted for chest pain and transient inferior ST-Elevation Myocardial Infarction (STEMI). She described chest pain on exertion for three days and chest pain at rest for one hour with a prompt relief after initial treatment in the ambulance. The patient had a history of coronary artery disease with PCI (drug eluting stents) in the LAD and RCA four years ago. The patient was taking aspirin, simvastatin, and ramipril. The initial electrocardiogram ([figure 1]) obtained in the ambulance demonstrated 2–3mm of ST-segment elevation in the inferior leads; and the patient’s chest pain was rated an 9 out of 10 at presentation, improving to two out of 10 after morphine, 5000 IE unfractionated heparin bolus, and aspirin 500 mg. Initial laboratory data showed a normal cardiac troponin. The second ECG ([figure 2]) repeated in the emergency room showed a spectacular regression of the ST-elevation. The patient was hemodynamically stable and nearly free of chest pain.
Angiography
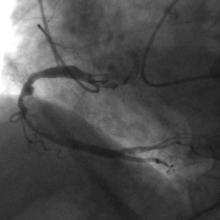
1) The RCA was an ectatic dominant vessel. A very large filling defect was visible in the middle portion of the vessel, involving also a previously implanted drug eluting stent associated with TIMI Flow III (Figure 3)
2) The left coronary artery showed normal left main coronary artery and some wall irregularities of the left anterior descending and the left circumflex (Figure 4)
2) The left coronary artery showed normal left main coronary artery and some wall irregularities of the left anterior descending and the left circumflex (Figure 4)
Procedure
1) The RCA was an ectatic dominant vessel. A very large filling defect was visible in the middle portion of the vessel, involving also a previously implanted drug eluting stent associated with TIMI Flow III (Figure 3)
2) The left coronary artery showed normal left main coronary artery and some wall irregularities of the left anterior descending and the left circumflex (Figure 4)
2) The left coronary artery showed normal left main coronary artery and some wall irregularities of the left anterior descending and the left circumflex (Figure 4)
Conclusion(s) / Result(s)
The patient was discharged on day 7 with ongoing treatment consisting of 10mg prasugrel, 300mg aspirin, 20mg pantoprazol, 5mg bisoprolol, 40mg atorvastatin, and 5mg ramipril. Six months later she remains free of symptoms.
Comments/Lessons
The no-reflow phenomenon still remains a very significant challenge for patients with acute myocardial infarction. Although there are a number of devices to treat the no-reflow phenomenon, it is still associated with poor prognosis. The phenomenon of no reflow is still poorly understood. Originally, it was thought that distal embolization of the plaque/thrombus following balloon inflation played a significant role in the development of no-reflow (1) The occurrence of acute no-reflow or slow-reflow phenomenon during PCI manifests itself as a sudden decrease in flow (to TIMI grade 0–1), a condition that is usually associated with clinical and ECG evidence of ischemia. This phenomenon is associated most frequently with PCI of SVGs and with PCI after STEMIs. (2,3,4) Prevention of no flow is a major challenge in acute STEMI patients and should include both pharmacological and mechanical interventions (5,6,7). In this patient treatment with optimal dual oral antiplatelet therapy and off-label use of low molecular weight heparin was able to eliminate completely the thrombus burden without any need for other interventions. We think that in a few patients like this one, a pharmacological approach with deferred intervention might be considered a better option compared with an ad-hoc intervention.
Conflicts of Interest
None






Comments