Obtaining Access for Transradial Catheterization in Pulseless Patients with Advanced Shock on ECMO
by
Pradeep K. Yadav
August 10, 2015Operator(s)
Pradeep K. Yadav, Giselle A. Baquero, Ian C. Gilchrist
Affiliation
Penn State University, Hershey, Pennsylvania
Facility / Institute
Penn State University, Hershey, Pennsylvania
Clinical History
A 49 year old male with severely reduced systolic function, day six post two vessel coronary artery bypass (CABG) had cardiac arrest after which two sternotomy explorations were performed. The patient was now in advanced cardiogenic shock on veno arterial ECMO, multiple inotropes, pressors and was referred to us for urgent coronary angiography of his bypass grafts. The patient had arterial cannula of the ECMO in the right femoral artery extending into the descending aorta. The left groin had several unsuccessful attempts at placing the arterial line during the cardiopulmonary resuscitation (CPR). The patient had no palpable pulses due to the continuous flow of the ECMO. Multiple blind attempts to place radial arterial lines in the intensive care unit (ICU) had failed.
Angiography
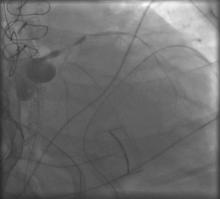
1) LMCA: 95% distal (Figure 1);
2) LAD: proximal 100%;
3) LCx: prox 80% diffusely diseased vessel;
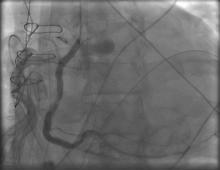
4) RCA: mid RCA: 50%; RCA PDA: 100% (Figure 2);
5) Ramus disease: 90%;
Coronary Artery Bypass Grafts:
6) LIMA to mid LAD: patent (Figure 3, Figure 4);
7) SVG to Ramus: patent (Figure 5);
8) L to R collaterals from distal LAD to the distal PDA.
2) LAD: proximal 100%;
3) LCx: prox 80% diffusely diseased vessel;
4) RCA: mid RCA: 50%; RCA PDA: 100% (Figure 2);
5) Ramus disease: 90%;
Coronary Artery Bypass Grafts:
6) LIMA to mid LAD: patent (Figure 3, Figure 4);
7) SVG to Ramus: patent (Figure 5);
8) L to R collaterals from distal LAD to the distal PDA.
Procedure
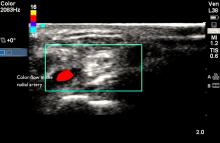
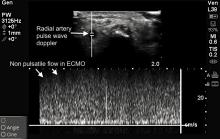
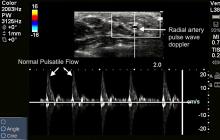
Two dimensional (2D) image with vascular ultrasound was used to identify and size the right radial artery. Non pulsatile flow was seen on color (Figure 6) and Doppler (Figure 7). Figure 8 demonstrates normal pulsatile flow in a hemodynamically stable patient. Under ultrasound guidance radial artery was punctured on first attempt and a 6 French sheath was placed.
Conclusion(s) / Result(s)
Coronary angiography was performed without difficulty and showed significant old disease in his native vessels and patent grafts. No intervention was required and patient was safely transported back to the ICU. With intensive support he stabilized and eventually underwent left ventricular assist device (LVAD) placement.
Comments/Lessons
Gaining access on the first attempt is optimal as repeated arterial trauma increases the risk for spasm. Therefore, careful vessel palpation and planning of arteriotomy puncture are critical to successful trans radial access (TRA).
Vascular ultrasound may help negotiate this challenge posed in radial access in conditions where the pulse is weak or absent. This may open the benefits of performing PCI via radial access, thereby exposing the patient to one less femoral artery puncture.
Vascular ultrasound may help negotiate this challenge posed in radial access in conditions where the pulse is weak or absent. This may open the benefits of performing PCI via radial access, thereby exposing the patient to one less femoral artery puncture.
Conflicts of Interest
None
We Recommend
Log in to post comments.



Chris Wong
Chris Wong