STEMI Patient with Large Thrombus in LM Treated with Full Dose Intracoronary Thrombolytic Therapy
by
Alghafek Almorraweh
March 24, 2014Operator(s)
Alghafek Almorraweh, MD Fadi Khazaal, MD
Affiliation
Al Bassel Heart Institute, Damascus, Syria
Facility / Institute
Al Bassel Heart Institute, Damascus, Syria
Clinical History
45 year-old male patient with no cardiac risk factors, presented following 4 hours of typical chest pain and shortness of breath. On physical examination, he had a BP= 85/60mmhg, HR= 90/min, and O2 Sat = 88%. He had fine bilateral basal crepitations on lung auscultation, and there was an evidence of S4 cardiac sounds. ECG showed ST elevations over leads II, III, aVF , aVR, V5 and V6, having the highest ST elevations amplitude in lead II at 4mm). Past medical history: Inferior ST elevation myocardial infarction (MI) 4 months before, treated with thrombolytic therapy. Treadmill stress test was done according to Bruce protocol for up to 10 minutes shortly after that, reaching stage 4, and the test was negative for any signs of ischaemia.
Angiography
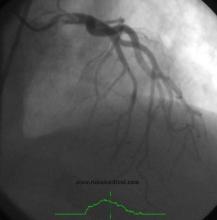
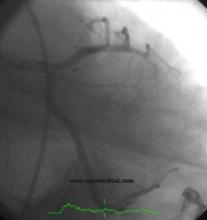
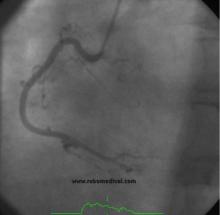
1) Left main coronary artery (LMCA): ostial large thrombus extending to the shaft inducing 95% stenosis (figure 1), (figure 2), (figure3)
2) Left anterior descending: normal
3) Left circumflex (Cx) : normal
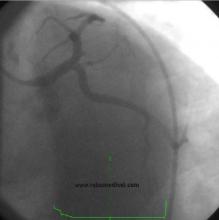
4) Right coronary artery (RCA): normal. (figure 4)
2) Left anterior descending: normal
3) Left circumflex (Cx) : normal
4) Right coronary artery (RCA): normal. (figure 4)
Procedure
After discussion with the cardiology team and the family, taking into consideration the size and the location of the thrombus and given that the patient had a recent inferior MI with angiographically completely normal RCA and Cx .
A 6Fr. Medtronic Launcher JL 4 guiding catheter was used to engage the LMCA. a bolus dose of Eptifibatide (integrilin) (180 mcg/kg) followed by 40mg (full dose) tenecteplase were given direct intracoronary within 15 minutes .
Follow up coronary angiography sequences were done after 1hour (figure 5 and figure 6), 3 hours (figure 7 and figure 8), and then 24 hours (figure9, figure10, and figure11) revealed complete resolution of the thrombus with TIMI III flow, having no distal embolisation or residual stenoses. Echocardiography on discharge showed an LVEF of 45% . Laboratory screening for hypercoagulable state revealed normal Protein C, Protein S, and Antithrombin III levels, with no Factor V Leiden mutation, except for an increase in the Homocysteine titer.
A 6Fr. Medtronic Launcher JL 4 guiding catheter was used to engage the LMCA. a bolus dose of Eptifibatide (integrilin) (180 mcg/kg) followed by 40mg (full dose) tenecteplase were given direct intracoronary within 15 minutes .
Follow up coronary angiography sequences were done after 1hour (figure 5 and figure 6), 3 hours (figure 7 and figure 8), and then 24 hours (figure9, figure10, and figure11) revealed complete resolution of the thrombus with TIMI III flow, having no distal embolisation or residual stenoses. Echocardiography on discharge showed an LVEF of 45% . Laboratory screening for hypercoagulable state revealed normal Protein C, Protein S, and Antithrombin III levels, with no Factor V Leiden mutation, except for an increase in the Homocysteine titer.
Conclusion(s) / Result(s)
Complete resolution of the thrombus with a TIMI 3 flow and no residual stenoses. Absence of hematoma at the femoral cannulation site with no hemorrhagic complications.
Comments/Lessons
For patient s with ACS who have large load thrombus in critical area (LM, ostial RCA),with high risk of embolization - either distal leading to no coronary reflow or migration towards the aortic lumen causing a potentially major vascular accident. intracoronary thrombolytic therapy with full dose tenecteplase may be one of successful optional treatment in the cathlab. Taking into consideration that position and successful not complicated puncture site are the cornerstone of this treatment option.
An elevated Homocysteine level could be a causative factor of intracoronary thrombus formation.
An elevated Homocysteine level could be a causative factor of intracoronary thrombus formation.
Conflicts of Interest
None







Comments