‘Acceptable Safety’ for LAA Closure Seen in a Real-World, All-Comers Registry
The data show that LAA closure with various devices can be done with a low major complication risk, one expert says.
ANAHEIM, CA—Closure of the left atrial appendage (LAA) using various devices can be achieved in real-world practice with a low rate of major periprocedural complications, a non-industry-sponsored German registry study shows.
Major device- and procedure-related complications occurring in the hospital, including severe bleeding and pericardial effusion requiring surgical or catheter-based treatment, were seen in 4.5% of patients, who had relatively high risks for stroke and bleeding at baseline, Thorsten Lewalter, MD, PhD (Hospital for Internal Medicine Munich South, Germany), reported last week at the American Heart Association 2017 Scientific Sessions.
That figure is higher than in some recent studies—which have shown rates below 3%—but is within previously reported ranges, indicating acceptable safety of the procedure, Lewalter told TCTMD.
Lewalter expressed some doubts about major complication rates below 3%, suggesting that selection bias and a focus only on experienced centers could be playing a role. “My feeling is that with 4% or 5%, we are very close to reality,” he said. “We had many centers involved, even those with a lower number [of cases], reflecting clinical practice in Germany.”
He added that in such a critically ill, elderly population, “you have to accept there is a small risk when you do the procedure.”
Still, Lewalter said, clinicians need to put in the effort to drive complications as low as possible to maximize the benefit of LAA closure. “That’s really crucial, and when this is done, we can downgrade to antiplatelet therapy and I think we will have a good therapeutic option in these high-risk patients.”
‘Very, Very Low’ MACCE Rates
The LAARGE registry, which involved 38 German hospitals, enrolled 641 patients with A-fib who underwent LAA occlusion between July 2014 and January 2016. Patients were considered high risk at baseline, with a median age of 77 years, a mean CHA2DS2-VASc score of 4.5, and a mean HAS-BLED score of 3.9. Follow-up will last for up to 5 years, but Lewalter presented in-hospital results only.
The main indication for the procedure was bleeding (79.4%), although referring physicians also frequently cited prior stroke/TIA (27.5%), patient choice (25.1%), and contraindication to oral anticoagulation (19.0%).
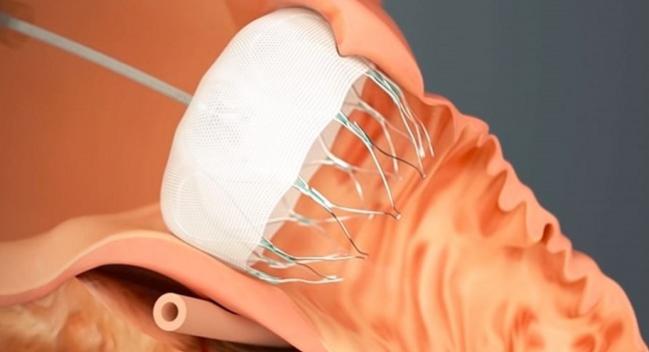
The most commonly used device was the Watchman (43.5%; Boston Scientific), followed by the Amplatzer Cardiac Plug (27.9%; St. Jude Medical), the Amplatzer Amulet (25.7%; St. Jude Medical), and others (2.8%).
The device was successfully implanted in 97.6% of cases, with a 5.2% rate of leaks smaller than 5 mm. Median procedure duration was 59 minutes.
Looking at in-hospital outcomes, four MACCE events—two deaths, a stroke, and an MI—occurred in three patients, for a rate of 0.5%. “I think this is very comparable to the reported low rate of events,” in other series, Lewalter said.
He said rates are slightly higher compared with prior studies for additional major complications, which included severe bleeding (1.1%), pericardial effusion requiring surgery (0.3%), pericardial effusion requiring catheter-based treatment (2.0%), arteriovenous fistula (0.9%), and dislocation requiring a separate revision (0.3%).
Commenting for TCTMD, Robert Sommer, MD (NewYork-Presbyterian/Columbia University Medical Center, New York, NY), said an important aspect of the findings is that even though overall complication rates were higher than in prior analyses, rates of the “really awful stuff” like deaths and strokes were “very, very low.”
Who Gets Treated, and How?
Lewalter and Sommer both indicated that LAA closure is primarily used in current practice for patients with a history of bleeding. “I think this is the area where the occluder has big potential,” Lewalter said.
In the United States, Watchman labeling states that eligible patients should have an elevated stroke or systemic embolism risk, should be deemed suitable for warfarin therapy, and should have an appropriate reason for seeking a nonpharmacologic alternative to warfarin. Recommended postprocedural therapy includes 45 days of warfarin.
But most patients currently treated in the United States, Sommer said, have a clear contraindication to oral anticoagulants—because of a prior intracranial hemorrhage or major GI bleed, for example. Thus, there is variation in practice in terms of antithrombotic therapy around the time of the procedure.
In the German registry, the proportion of patients taking oral anticoagulation fell from 61.2% before the procedure to 12.7% at discharge, whereas the rate of antiplatelet treatment jumped from 34.4% to 96.1%, including a dual antiplatelet therapy rate of 86.4%.
Lewalter noted that postprocedural antithrombotic therapy varied widely, and Sommer said that is consistent with what’s happening in the United States. Some patients are treated with non-vitamin K antagonist oral anticoagulants (NOACs) instead of warfarin after the procedure, whereas some are discharged on single or dual antiplatelet therapy or, in extreme cases, nothing at all. Both Lewalter and Sommer said more randomized data would be helpful in this space, and Sommer said the ongoing ASAP-TOO trial should provide some guidance.
Photo Credit: Adapted from http://www.watchman.com
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Lewalter T. Interventional occlusion of left atrial appendage in patients with atrial fibrillation: study design and acute procedural outcome of occluder implantation in the LAARGE registry. Presented at: American Heart Association 2017 Scientific Sessions. November 12, 2017. Anaheim, CA.
Disclosures
- Lewalter reports serving on the speakers’ bureau for Abbott and Boston Scientific.


Comments