After TAVI, Single Antiplatelet Better Than Dual: TRITAVI Registry
No matter whether patients had CAD or not, the simpler regimen was linked to less mortality and major bleeding at 6 months.
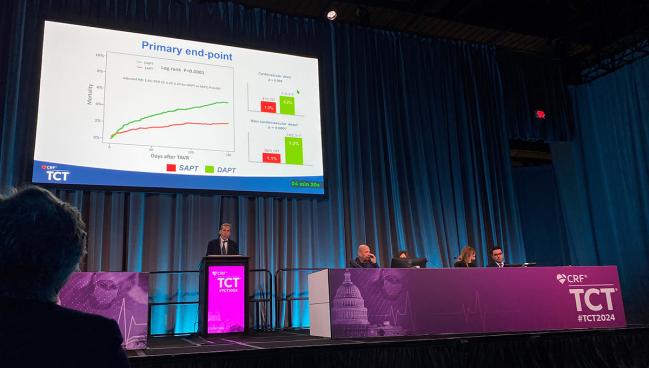
WASHINGTON, DC—Compared with dual antiplatelet therapy (DAPT), taking a single antiplatelet following TAVI is associated with a lower rate of all-cause mortality and major bleeding at 6 months, according to new registry data.
The findings from TRITAVI are in line with the POPular TAVI trial as well as previous retrospective data indicating that most TAVI patients do well with single antiplatelet therapy. Exceptions are those at high risk of ischemic events and those who need to keep taking DAPT for established CAD.
The 2021 European guidelines for valvular heart disease give a class 1, level of evidence A recommendation for lifelong single antiplatelet therapy with aspirin of clopidogrel for TAVI patients with no baseline need for oral anticoagulation. The 2020 US guidelines give a class IIa, level of evidence B-R recommendation for aspirin monotherapy following TAVI “in the absence of other indications for oral anticoagulants.
But notably, said Francesco Pelliccia, MD (Sapienza University of Rome, Italy), who presented the TRITAVI results last week at TCT 2024, “we observed a huge variability in antithrombotic protocols among the 20 participating treatment centers.” This, he added, demonstrates a need for more conclusive evidence in this space.
TRITAVI Findings
The study included 5,514 patients who underwent TAVI among 20 European centers from 2012 to 2022. Researchers excluded patients who had been previously on anticoagulation, had nonfemoral TAVI, experienced procedural complications, or had a history of ACS or PCI within the prior year.
A total of 3,197 patients received single antiplatelet therapy (mean age 81.3 years: 50.8% male) and 2,317 had DAPT (mean age 81.8 years; 45.2% male). The DAPT cohort had more hypertension, smoking, CAD, prior MI, prior PCI, and PAD; but less often reported NYHA class III or IV symptoms and had less chronic obstructive pulmonary disease.
Just under half of each group received a CoreValve device (Medtronic), with 27.1% and 37.1% of the single and dual antiplatelet arms having an Edwards Lifesciences valve—Pelliccia didn’t specify which iteration—and 24.1% and 15% receiving a different TAVI device. Procedural characteristics were similar between the cohorts, but there were more vascular complications (8.6% vs 4.6%) and blood transfusions (18.6% vs 11.4%) in the DAPT vs single therapy patients (P < 0.001 for both).
All-cause mortality was about one-third lower with single antiplatelet therapy compared with DAPT at 6 months (adjusted HR 1.65; 95% 1.22-2.23), with significant drops in both cardiovascular (1.3% vs 2.2%; P = 0.008) and noncardiovascular death (1.1% vs 3.2%; P = 0.001).
On multivariate analysis, individual predictors of all-cause mortality included DAPT use (HR 1.65; 95% CI 1.22-2.23), NYHA class III-IV (HR 1.56; 95% CI 1.10-2.21), and presence of CAD (HR 1.40; 95% CI 1.05-1.87). A subanalysis looking separately at patients with and without known CAD confirmed the primary findings.
The secondary endpoint of major ischemic events trended lower for single versus dual antiplatelet therapy (0.4% vs 0.7%; P = 0.07), but major bleeding was significantly lower with the former (0.5% vs 1.3%; P = 0.001).
Pelliccia reported that temporal trends in antithrombotic prescriptions remained “constant” throughout the study period, with single antiplatelet therapy more often prescribed than DAPT by referring physicians. The “slight increase” in single therapy observed in the last 2 years likely reflects the effect of the POPular TAVI trial, he said. Mortality was consistently higher for patients receiving DAPT compared with a single agent.
Open Questions
What remains unknown is whether “a potent P2Y12 inhibitor as a single strategy works better [than aspirin or clopidogrel] in order to not only to decrease the risk of bleeding, but also to protect for ischemic events,” said panelist Victor Alfonso Jimenez Diaz, MD (Hospital Alvaro Cunqueiro, University Hospital of Vigo, Spain). “Also, going beyond that, trying to avoid subclinical leaflet thrombosis in the valve, because this is an issue that we are discovering here and we don't know, actually, if the antiplatelet therapy plays a role regarding this event.”
Pelliccia said he agreed, noting his surprise that patients with known CAD in the study still see benefit from treatment with a single agent. “In the real world, often physicians prefer to protect their own patient [by prescribing DAPT] when they have a TAVR and they are a coronary artery disease patient,” he said. “But this is wrong. What our data show is that this should not be our default approach.”
Panelist Soledad Ojeda, MD, PhD (Hospital Universitario Reina Sofía, Cordoba, Spain), however, said she still has doubts about the ability to prevent ischemic events with single therapy. “Obviously the risk of bleeding is lower when you use only single antiplatelet therapy,” she said, noting that this wasn’t observed for ischemic events.
“You make a good point,” Pelliccia said. But “this means that we can protect our patients with single antiplatelet treatment.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Pelliccia F. Antiplatelet therapy and all-cause mortality after transcatheter aortic valve replacement. Presented at: TCT 2024. October 27, 2024. Washington, DC.
Disclosures
- Pelliccia reports no relevant conflicts of interest.






Comments