AI in Pulmonary Embolism: ‘Transformative’ for Patient Care
Two physicians at ISET 2024 shared their firsthand impressions of what AI can bring to PE diagnosis, triage, and treatment.
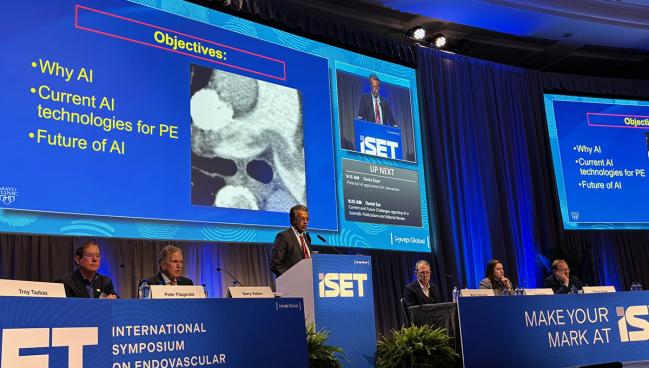
MIAMI BEACH, FL—Pulmonary embolism (PE), an often-deadly condition that’s best served by a multidisciplinary approach to care, is the perfect target for artificial intelligence (AI), according to experts at last week’s ISET meeting. Clinicians at some centers have already begun to apply this rapidly developing technology to streamline the management of PE patients, and say they’re learning as they go.
“AI is everywhere,” Sanjay Misra, MD (Mayo Clinic, Rochester, MN), told attendees of the packed ISET Town Hall session. “It’s ubiquitous, and I think it’s really important for us in healthcare to start looking at it and understanding how we’re going to use it.” That day has come in many large health systems, where AI is harnessed for stroke triage, image analysis, and more, he said.
Pulmonary embolism, in particular, stands out as an area of clinical need, Misra said. “PE is a huge problem.” There are 900,000 cases of PE each year in the United States, leading to 300,000 deaths annually, with a stark rural/urban divide in mortality risk.
Increasingly, academic medical centers approach the challenges of PE through pulmonary embolism response teams (PERTs). This strategy isn’t universal, however, and the centers that lack PERTs could especially stand to benefit from AI tools, said Robert Lookstein, MD (Icahn School of Medicine at Mount Sinai, New York, NY), not only for diagnostics but also for connecting and informing caregivers across disciplines.
Lookstein, in an ISET session devoted to venous clot management, had the opportunity to discuss his own firsthand experiences with AI in PE. He described himself as an “absolute zealot” about the technology’s potential. “Literally, this is where we are going to go for treating PE, and this is in my opinion the future of advanced diagnosis and triage of all cardiovascular emergencies,” said Lookstein.
For him and his colleagues at Mount Sinai, using AI for PE “has been such a transformative experience,” one that he wants to share with other centers, Lookstein told TCTMD. “Everyone on our clinical team, on our PERT, can’t imagine going back to what it was like before we had this. Everybody agrees that we are triaging patients much more rapidly. We’re identifying who needs escalation in care. We’re identifying disposition. We have proven that we’ve reduced length of stay. Now, we need to prove that we’re improving outcomes.”
What It Does
Admittedly, AI has been around in healthcare for some time, Lookstein said, but it’s only within the past several years that platforms like Aidoc aiOS, RapidAI, and Viz.ai debuted in PE care. Their smartphone apps, as a first step, could rapidly identify PE based on an initial CT, then “ping the physician and notify them” when the PE is diagnosed. More complicated has been fine-tuning these algorithms to winnow down the alerts to those that are most actionable, drawing a distinction between patients who require intervention and those who can be medically managed based on factors like RV/LV ratio, biomarker elevations, and ECG changes.
Then, the app must connect all the clinicians involved, Lookstein said, such that “regardless of whether somebody is in the emergency room, on the floor, in the operating room, cath lab, etc, that everybody is communicating about this urgent diagnosis at the exact same time, sharing their opinions and their concerns about where the patient should be triaged to.” And finally, this information needs rapid integration with the patient’s electronic health record (EHR), he said.
It's taken time, and a lot of work, to reach the stage where all of these AI-based functions are available for clinical use, he added.
Everybody is communicating about this urgent diagnosis at the exact same time, sharing their opinions and their concerns about where the patient should be triaged to. Robert Lookstein
Misra also called out the complexity of care for acute PE. Patients pass through many steps—with many different components—from the initial suspicion of disease to diagnosis on CT, creation of the radiology report, and pursuit of other testing that’s relevant to PE treatment, he noted.
For all members of the team to be informed, there must be ways of “pulling this data out of silos . . . and coordinating a story about the patient and what’s best for the patient,” said Misra. “And this can be hard.”
According to Lookstein and Misra, both Mount Sinai and the Mayo Clinic are using the Aidoc aiOS system, whose features for PE include a smartphone app that provides PERT alerts, mobile image viewing, RV/LV ratio-based risk stratification, EHR integration, and a platform for chats across departments. Additional dashboards offer center-specific details on things like turnaround time and percent positives. “If you’re a large healthcare system, this kind of data may be valuable for you to understand workflow, diagnoses, and communication,” Misra said.
“It’s amazing how automatically the data is aggregated,” Lookstein concurred. The numbers that come out of that can be used to create reports on a weekly, monthly, or quarterly basis for sharing with PERT members, said Lookstein. At Mount Sinai, they’ve also provided the AI vendor with real-time feedback that’s improved diagnostic accuracy: the negative predictive value has reached nearly 99%.
Money and Knowledge
The potential to save money, by targeting the right resources to the right patients, is another thing on everyone’s minds.
Misra, looking forward, cited a recent American Heart Association scientific statement that calls for “value creation” as artificial intelligence is applied in cardiovascular imaging. “What we don’t want to do is drive up the cost of medicine,” he urged. Additional elements include the need to better standardize data collection from disparate sources and to reduce disparities in care, as well as the requirement for adequate IT infrastructure and the ability to safely deal with patient privacy.
The hype around artificial intelligence is high but justified, Misra noted. “I would encourage those of you that are interested: start engaging with AI because you are at the right time.”
What we don’t want to do is drive up the cost of medicine. Sanjay Misra
Gradually, studies are documenting what AI adds to PE care, said Lookstein. “There is research, but honestly in my opinion this field is moving so fast it’s hard to generate data that’s reflective of what’s happening now.”
AI isn’t just under study itself: it’s also bolstering the research infrastructure of the hospitals that use it. Lookstein said the PERT Consortium has been working with the various AI vendors to optimize their products and ensure they are consistent among each other. Beyond this, though, “the PERT Consortium has been committed, since its inception, to supporting, promoting, and advocating for prospective research in this space,” he said. By tracking detailed information over time, AI “allows you to make sure that your research site is ideally suited to screen every single patient, not miss one, and allow them to be screened for participation in these pivotal, prospective trials.”
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Misra S. AI in pulmonary embolus diagnosis and treatment. Presented at: ISET 2024. January 23, 2024. Miami Beach, FL.
Lookstein R. Artificial Intelligence and acute pulmonary embolism. Presented at: ISET 2024. January 24, 2024. Miami Beach, FL.
Disclosures
- Misra reports receiving research grants from the National Institutes of Health as well as the Regenerative Minnesota Medicine Grant; serving on data safety and monitoring boards for Humacyte and Penumbra; consulting for Medtronic; being the founder of Pavaj Vascular; and holding equity in Inova Vascular.
- Lookstein reports serving on the advisory boards of Boston Scientific and Medtronic; being a consultant to Penumbra and Neptune Medical; serving on clinical events committee/data safety and monitoring boards for Intact Vascular (Philips), Shockwave, Trireme, and Thrombolex; being on the speakers bureau of Abbott Vascular; being an equity shareholder of Truvic and Innova Vascular; and receiving research support from Philips Healthcare, Spectranetics, Terumo, Boston Scientific, INARI, Penumbra, Ethicon, Walk Vascular, and Black Swan.





Comments