With ANOCA, Better to Test Coronary Function in Multiple Vessels
Casting a wide net allows for better diagnostic yield and targeted care in patients with stable angina but no obstructive CAD.
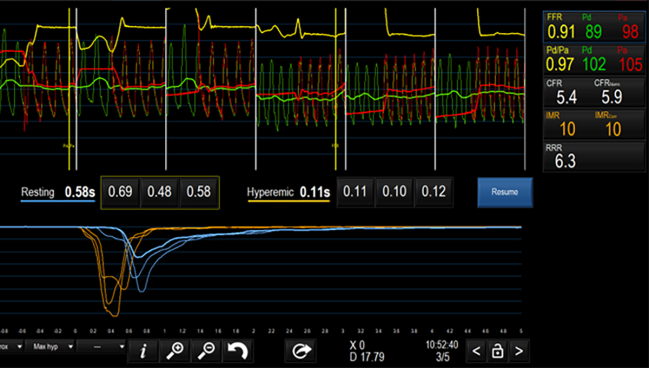
Photo Credit: Adapted from Prasad M. Case in a Box: Step-by-step Approach to Assessment of Microvascular Disease in an INOCA Patient. Presented at: TCT 2023. San Francisco, CA.
For patients with stable angina and nonobstructive coronary arteries (ANOCA), casting a wider net when performing invasive coronary function testing (CFT) offers an increased diagnostic yield, a new prospective study suggests.
Multivessel CFT, compared with single-vessel testing only, increased the proportion of patients diagnosed with coronary vasomotor dysfunction, coronary artery spasm, and coronary microvascular dysfunction (CMD), researchers report in a study published recently in JACC: Cardiovascular Interventions.
Already, they say, invasive CFT using acetylcholine to diagnose coronary spasm and adenosine to evaluate the microcirculation is the “gold standard” for evaluating ANOCA patients, with the goal of categorizing disease into distinct endotypes. “This classification allows clinicians to tailor therapy to individual patients, an approach that has [been] shown to improve angina status and quality of life,” Rajan Rehan, MD (Royal Prince Alfred Hospital, Sydney, Australia), and colleagues write. For instance, patients with epicardial or microvascular spasm would take a calcium channel blocker as the first-line drug, and those with CMD would first take a beta-blocker in combination with ACE inhibitors or ARBs and statins.
In today’s practice, just a single coronary vessel is typically evaluated with such testing, the researchers note. “However, the potential diagnostic benefits of extending CFT to evaluate multiple coronary territories in these patients are unclear.”
Speaking with TCTMD, Rehan observed that coronary angiography, when used as a diagnostic test, examines multiple arteries. This begs the question: why shouldn’t that be the case with CFT? “That’s really what triggered [our study],” he said.
He acknowledged that CFT is currently underused as it is. Going beyond just one vessel only adds 15 minutes of time to the procedure, he pointed out. “In the big scheme of things, you’re already there. . . . Once you’re comfortable with the process already, then doing it in another vessel is actually quite quick.”
Commenting on the study for TCTMD, Javier Escaned, MD, PhD (Hospital Clínico San Carlos, Madrid, Spain), observed, “To me, the first take-home message is that vasomotor disorders are much more frequent than has been suspected . . . and the more you look into it, the more time you spend looking into different arteries, the more chance you will spot that abnormal vascular function. I think that is probably what this study is going to contribute, mainly, to the body of knowledge, saying, ‘Listen, this is something you can no longer ignore.’”
Different Answers in Different Arteries
For the observational study, the investigators enrolled 80 ANOCA patients (mean age 57.8 years; 60% women) who underwent CFT. The choice of which vessel to assess first was at operator discretion, after which CFT was performed in the remaining major epicardial coronary arteries.
Multivessel testing, compared with single-vessel CFT, increased the proportion of patients diagnosed with coronary vasomotor dysfunction (86.3% vs 68.8%; P = 0.0005), coronary artery spasm (60.0% vs 47.5%; P = 0.004), and CMD, defined as abnormal index of microcirculatory resistance and/or coronary flow reserve (62.5% vs 36.3%; P < 0.001).
With coronary artery spasm, most cases were found in the left coronary system, but one in five cases were isolated right coronary spasm. A little more than half (52.5%) had epicardial spasm, most with a diffuse pattern, and 7.5% had microvascular spasm.
With CMD, single-vessel dysfunction was most common, but 18.8% of patients had two affected vessels and 10% had three. Cases were equally likely to occur in the left anterior descending, left circumflex, and right coronary arteries. Forty percent of the patients with CMD had an elevated index of microcirculatory resistance, 30% had reduced coronary flow reserve, and 30% had both. On the Seattle Angina Questionnaire, patients with multivessel CMD had significantly worse angina quality-of-life scores than did those with single-vessel CMD.
“These findings suggest that regional variations in coronary vasomotion and microvascular function may exist, and single-vessel CFT could result in an underdiagnosis, ultimately affecting clinical management and patient outcomes,” Rehan et al conclude. Next up, they add, clinical trials should investigate the prognostic significance of multivessel CFT in ANOCA patients as well as the strategy’s therapeutic potential.
Importantly, real-world use of multivessel CFT would be less onerous than what’s described in their paper, Rehan stressed.
“In this study, we checked all vessels on baseline, whether we found a diagnosis in the first one or not,” he explained. In actual practice, “if we don’t find a diagnosis in the first vessel, yes, we do proceed to the other vessels, because now we know we might find a diagnosis. I think that’s all we’re advocating for, not to just check all three vessels for no reason.”
When a diagnosis isn’t clear on the first try, not pursuing answers with additional testing is doing patients a disservice, Rehan added.
Escaned pointed to another recent paper, published in the Journal of the American College of Cardiology, showing that ANOCA patients who developed ischemia on exercise stress testing were also more likely to have underlying CMD identified by invasive coronary physiological assessment using adenosine and acetylcholine. “In that context, I think that is where this paper is one more piece of evidence saying, ‘Listen, this is something important, you have to look for it, and you have to consider [microvascular dysfunction]” in the diagnostic workup.
Coen K.M. Boerhout, MD (Amsterdam UMC, the Netherlands), and Tim P. van de Hoef, MD, PhD (UMC Utrecht, the Netherlands), in an accompanying editorial, point to the clinical relevance of the study’s topic. Up to half of patients undergoing coronary angiography for suspected myocardial ischemia ultimately will be found to lack obstructive disease, they note, and other studies have shown that routine CFT on top of angiography in ANOCA patients reveals that over two-thirds have some form of coronary vasomotor dysfunction.
“Importantly, early detection and distinction of the specific endotype by means of the coronary function test and subsequent stratified treatment is shown to improve quality of life in ANOCA patients considerably,” they concur.
Studies like the current one are persuasive that “the more, the merrier” applies to diagnostic approaches in the cath lab, the editorialists add, and “will serve as the basis to develop an optimal coronary function testing protocol, lowering thresholds for comprehensive testing and increasing the diagnostic yield for patients with ANOCA.”
For Escaned, this paper, advocating for multivessel CFT, is more likely to be embraced by centers already regularly testing coronary function and looking for vasomotor disorders, but may be “a bridge too far” for centers not currently equipped to perform these tests. The larger problem, he added, is that coronary flow disorders and microcirculatory dysfunction are not much on the radar of clinicians more broadly. The current paper serves as a reminder for the need to look for the problem in the first place, and to do so thoroughly.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Rehan R, Wong CCY, Weaver J, et al. Multivessel coronary function testing increases diagnostic yield in patients with angina and nonobstructive coronary arteries. J Am Coll Cardiol Intv. 2024;17:1091-1102.
Disclosures
- Rehan is supported by the National Health and Medical Research Council Postgraduate Scholarship.



Comments