Cardiac MR Noninferior to CT for TAVI Planning, Small RCT Shows
The findings could unlock an alternative for patients with CKD wanting to avoid contrast and radiation, the authors say.
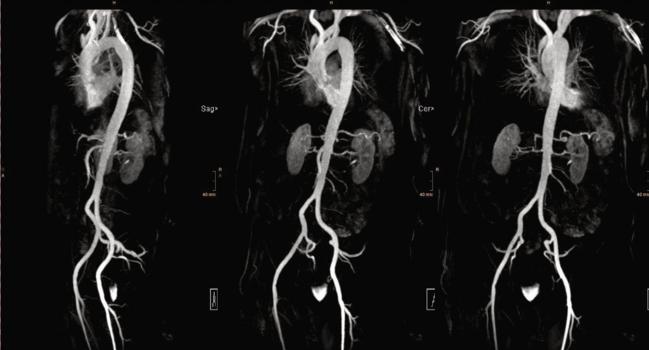
Photo Credit: Sebastian J. Reinstadler
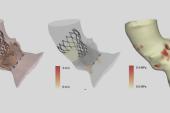
Using cardiac magnetic resonance (CMR) imaging to guide TAVI cases is noninferior to the more common approach of preprocedural computed tomography with regard to device implantation success, according to new randomized data.
While CT should remain the gold standard in most TAVI patients, the authors say, the data unlock a potential new radiation-free alternative especially for those with chronic kidney disease (CKD)—who make up between one-third and one-half of the TAVI population—who may be sensitive to the use of iodinated contrast media.
“For most of the patients, CT is really perfect,” senior author Sebastian J. Reinstadler, MD, PhD (Medical University of Innsbruck, Austria), told TCTMD. “It is fast, and it delivers accurate results, but there may be situations in everyday clinical practice where CMR could really offer some advantages.” The results of this trial offer the “first randomized evidence to justify safe use of CMR in this situation,” he added.
TAVR-CMR findings
For the TAVR-CMR trial, which was published last month in Circulation, Reinstadler, Martin Reindl, MD, PhD (Medical University of Innsbruck, Austria), and colleagues randomized 380 TAVI candidates from their institution to have their procedure guided by either CMR (n = 191) or CT (n = 189) between September 2017 and December 2022.
Ultimately, 72.3% of the CMR group and 68.3% of the CT group underwent TAVI, including 19 with protocol deviations. Implantation success at discharge (primary outcome) was achieved in 93.5% and 90.7% of those who had their procedures guided by CMR and CT, respectively (between-group difference 2.8%; 90% CI -2.7 to 8.2%; P < 0.01 for noninferiority). The per protocol analysis met noninferiority criteria as well (between-group difference 2.0%; 90% CI -3.8 to 7.8%; P < 0.01 for noninferiority).
Mean scan time was longer in the CMR group compared with CT (35 vs 10 minutes), but the CT group had to contend with exposure to contrast (median volume of 80 mL) and radiation (median dose length product of 520 mGy*cm).
Secondary safety outcomes were comparable between the groups, with the exception of stroke or TIA and need for permanent pacemaker implantation occurring more frequently following CT-guided TAVI.
While CMR requires additional education and experience, and might also take longer and be more costly than CT, Reinstadler said, “if you do cardiac magnetic resonance in your hospital, you should be able to establish this protocol.”
He would like to see the findings confirmed in larger, multicenter trials. Down the line, additional studies using CMR to do myocardial tissue characterization could potentially help with severity assessment of the aortic stenosis, Reinstadler said. “You could see the consequences of the stenosis for the myocardium and decide if the patient is, for example, symptomatic, whether it is already time to intervene or whether careful watchful waiting would be more appropriate. And then you [would] also have, already, the information for planning the intervention.”
CMR Limitations
Speaking with TCTMD about the study, João L. Cavalcante, MD (Minneapolis Heart Institute Foundation, MN), said he wasn’t entirely convinced that CMR can compete with CT for TAVI planning.
The risk of contrast-induced nephropathy following CT has gone down over time due to better hydration practices, improved scanners, lower contrast volumes, and a better understanding of patient risk factors, he explained. “It is good that CMR is a proposition here, but as much as I love CMR and I [use it for different applications], it has some limitations.”
Chief among them, Calvalcante said, is CMR’s inability to see calcium so as to identify the best landing zone on the annulus. “The amount of calcification of the valve we can indirectly assess, but that is not ideal,” he said, adding that CMR also won’t contribute information about calcification of the femoral vessels that might benefit from lithotripsy.
It is “good to see” that CMR can assess suitability of TAVI, but this was not unexpected, Cavalcante said. “There does not seem to be harm by using CMR as an alternative.” Also, it might not be feasible at all centers, he added. “For all those reasons, I think it is a nice development in the right direction, but I don't think that this will be changing practice substantially.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Reindl M, Lechner I, Holzknecht M, et al. Cardiac magnetic resonance imaging versus computed tomography to guide transcatheter aortic valve replacement (TAVR-CMR): a randomized, open-label, non-inferiority trial. Circulation. 2023;Epub ahead of print.
Disclosures
- Reindl, Reinstadler, and Cavalcante report no relevant conflicts of interest.



Comments