Chronic HF Patients Needing CRT Fare Better With LBB Pacing: HeartSync-LBBP
Despite the randomized trial showing a difference in outcomes, more data are needed before changing practice, says one expert.
VIENNA, Austria—Patients with chronic heart failure who require cardiac resynchronization therapy (CRT) fare better when left bundle branch (LBB) pacing is used over traditional biventricular (BiV) pacing, according to the randomized HeartSync-LBBP trial.
Patients who received LBB pacing had greater improvements in QRS duration and left ventricular function and size, as well as better clinical outcomes, Xueying Chen, MD, PhD (Zhongshan Hospital, Fudan University, Shanghai, China), reported here at the European Heart Rhythm Association Congress 2025.
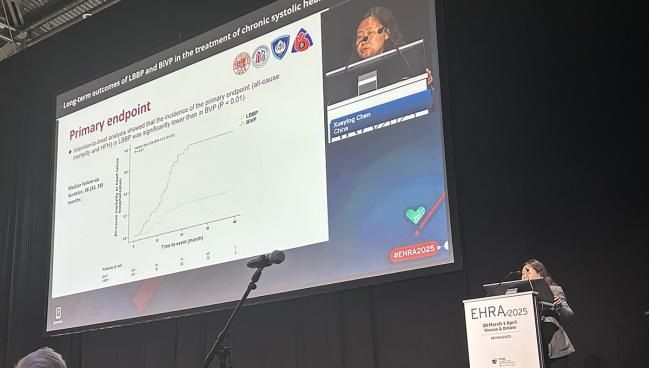
Through 3 years of follow-up, the primary composite endpoint of all-cause mortality or heart failure hospitalization was reduced by a relative 74% with LBB versus BiV pacing.
“We demonstrate LBB pacing [provides] a greater electrical and mechanical and echocardiographic improvement than BiV pacing in heart failure patients with LBBB [left bundle branch block], and it is potentially an alternative to BiV pacing,” Chen concluded.
Prior evidence from observational studies and a small pilot RCT had hinted that LBB pacing provides better outcomes than BiV pacing for patients with heart failure and LBBB treated with CRT but, until now, there had been no large randomized trials comparing longer-term results with the two approaches. In the absence of conclusive randomized data, BiV pacing remains the standard approach. Pacing and CRT guidance from the European Society of Cardiology, for instance, states that “especially in CRT candidates with LBBB, biventricular pacing has more solid evidence of efficacy and safety, and therefore remains first-line therapy.”
HeartSync-LBBP
The single-blind HeartSync-LBBP trial, conducted at six Chinese centers, included 200 patients (mean age about 65 years; 68% men) who had chronic systolic heart failure, LBBB, an LVEF of 35% or less, and NYHA class II-IV symptoms despite being on guideline-directed medical therapy (GDMT) for at least 3 months.
Most patients (83%) had nonischemic cardiomyopathy, with a mean LVEF of 28%. More than 90% of participants were taking three-component GDMT consisting of an ACE inhibitor/ARB/angiotensin receptor-neprilysin inhibitor, a beta-blocker, and spironolactone.
There was some crossover in the trial, with six patients assigned to the BiV group getting LBB pacing due to unfavorable venous anatomy (n = 4), high pacing threshold (n =1), and phrenic nerve stimulation (n = 1). In addition, two patients assigned to LBB pacing crossed over to the BiV group due to a failure to screw in the lead.
Through a median follow-up of 36 months, QRS duration improved in both arms of the trial, although the narrowing was greater with LBB pacing—at the end of follow-up, mean QRS duration was 120.6 ms in that arm and 137.4 ms in the BiV arm (P < 0.01). Moreover, patients in the LBB pacing group—compared with BiV pacing—had a greater mean LVEF at 3 years (47.3% vs 41.5%), and lower LV end-systolic diameter (41.8 vs 48.1 mm) and LV end-diastolic diameter (55.3 vs 60.3 mm; P < 0.01 for all).
Though there was no difference between the LBB and BiV pacing groups in the proportion of patients considered responders based on a 5% or greater improvement in LVEF (90% vs 84%; P = 0.21), there were more super responders—an increase of at least 15% or an improvement to 50% or greater—in the LBB pacing group (65% vs 44%; P < 0.01).
There advantages for LBB pacing were accompanied by better clinical outcomes, with a rate of all-cause mortality or heart failure hospitalization of about 8% versus 32% with BiV pacing (HR 0.26; 95% CI 0.12-0.57). Results were similar across subgroups. The difference was driven by a reduction in heart failure hospitalization (HR 0.23; 95% CI 0.10-0.52), with no gap between groups in mortality (HR 0.40; 95% CI 0.08-2.04).
Chen acknowledged some limitations of the trial, including the high percentage of men and patients with nonischemic cardiomyopathy and the inclusion of Chinese patients only, which may impact generalizability; the involvement of centers that were experienced in LBB pacing; and the lack of preprocedural MRI data, complicating the analysis of scar and etiology.
Risk of bias may be considerable . . . in this unblinded trial. Jens Cosedis Nielsen
Discussing the results after Chen’s presentation, Jens Cosedis Nielsen, MD, PhD (Aarhus University Hospital, Denmark), noted that HeartSync-LBBP is the largest trial to explore this topic and shows a “quite amazing difference” in the primary composite endpoint.
However, he raised some questions to consider when interpreting the results, including the relatively low rate of mortality in the study population (about 1% per year). “At least in our institution this is a little higher, so I would question how severe this heart failure was,” Nielsen said.
He also highlighted uncertainties involving blinding, the definition of heart failure hospitalization, adjudication of outcomes by an endpoint committee, measures to minimize the risk of bias when assessing responder status, and others.
Though there was a large difference in clinical outcomes, “risk of bias may be considerable . . . in this unblinded trial,” Nielsen said. “Thus, still, more data are needed before changing our practice to left bundle branch pacing in heart failure with LBBB.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Chen X. Long-term outcomes of LBBP and BVP in chronic systolic heart failure with LBBB: a multicenter, prospective, randomized, controlled trial (HeartSync-LBBP trial). Presented at: EHRA 2025. March 30, 2025. Vienna, Austria.
Disclosures
- Chen and Nielsen report no relevant conflicts of interest.





Comments