CMR Perfusion Imaging Holds Its Own Against Invasive Approach to Managing Stable Angina
The trial reconfirms the role of stress testing as an alternative to angiography plus FFR for guiding initial management decisions, one expert says.
WASHINGTON, DC—A noninvasive approach to guiding initial management decisions in patients with stable angina that employs stress cardiovascular magnetic resonance (CMR) perfusion imaging provides outcomes similar to those seen with a more invasive approach, the MR-INFORM trial shows.
At 1 year, the rate of MACE (all-cause death, nonfatal MI, or TVR) was 3.3% following CMR guidance and 3.9% following invasive angiography plus fractional flow reserve (FFR), a nonsignificant difference (P = 0.62), Eike Nagel, MD (University Hospital Frankfurt, Germany), reported at the American College of Cardiology 2017 Scientific Session here.
Outcomes were similar despite the fact that CMR guidance was associated with a lower revascularization rate (36.0% vs 44.2%; P = 0.0053).
As a means of guiding the initial management of patients with stable angina and an intermediate-to-high risk of CAD, noninvasive CMR perfusion imaging is noninferior to a strategy with invasive angiography supported by FFR during 1-year follow-up, Nagel concluded.
Commenting for TCTMD, Pamela Douglas, MD (Duke University, Durham, NC), said that some physicians have argued that the approach to managing these patients should involve a direct-to-catheterization strategy because of the imprecision of noninvasive tests. But this study, she said, “reconfirms the role of stress testing as being viable and in some ways preferable” to more invasive approaches.
The study investigators did not yet release an economic analysis, but Douglas said the noninvasive approach would be more cost-efficient than the FFR-guided strategy, citing the lack of a difference in outcomes, the avoidance of revascularization procedures in the CMR group, and the lower cost of performing MRI versus doing a catheterization.
Though the study supports the safety and efficacy of using CMR guidance in this population, Douglas added that it does not inform the choice between the various noninvasive modalities that are available.
Best Invasive vs Best Noninvasive Testing
Nagel said MR-INFORM was designed to compare what is considered the best invasive strategy for initial management of patients receiving optimal medical therapy for stable angina—angiography with FFR—with what seems to be the best noninvasive approach. CMR perfusion imaging has shown the highest accuracy among noninvasive tests, doesn’t require radiation, and provides information on anatomy, function, and myocardial structure in a single session, he said.
The trial, conducted at 16 sites in Europe and Australia, randomized 918 patients with stable angina (Canadian Cardiovascular Society grade II or III) and an intermediate-to-high risk of CAD, demonstrated by having at least two risk factors or a positive exercise treadmill test. All patients received optimal medical therapy to control risk factors.
In the invasive group, patients underwent angiography with FFR performed in all arteries that were larger than 2.5 mm and contained stenosis of 40% to 95%. Revascularization was recommended when FFR values were below 0.8.
In the noninvasive group, patients were imaged with a 1.5T MR scanner, with cine imaging, adenosine stress/rest perfusion imaging, and late gadolinium enhancement. A transmural defect or subendocardial defect found in more than two segments or in two adjacent slices triggered a recommendation for revascularization.
The percentage of patients who had positive results on both functional and anatomical testing—indicating significant CAD—was higher in the patients receiving FFR guidance (47.5% vs 41.5%; P = 0.0047), in whom the revascularization rate was also higher.
“In and of itself, we don’t know if that’s a good thing or a bad thing, except we do know that it didn’t improve outcomes to have those extra procedures,” Douglas commented. “It certainly raises the question of whether all those PCIs were necessary.”
Moreover, she said, the findings from MR-INFORM combined with those from two trials comparing FFR and instantaneous wave-free ratio (iFR) that were also presented at the meeting—DEFINE-FLAIR and iFR-SWEDEHEART—raise some questions about FFR. In all three trials, FFR identified more obstructive lesions and was associated with more revascularization versus the comparators.
“The reason I bring that up is that perhaps we’re seeing some of the flaws of FFR now that we’re looking thoughtfully and carefully at alternative approaches. And I say that very cautiously,” Douglas stated. “But I think there’s some evidence that FFR may overestimate lesion significance in the iFR trials as well as in the MR-INFORM trial.”
Those findings are “very hypothesis-generating,” she stressed, adding, “Certainly I’m not one to condemn FFR or to say that we shouldn’t be using it in our cath labs to evaluate lesions, particularly in the absence of anything better in clinical use.” It is, however, an issue that deserves attention moving forward, she said.
Findings ‘Not Very Surprising’
Chetan Shenoy, MBBS (University of Minnesota, Minneapolis), who was not involved in the study, told TCTMD, “As someone who does stress CMR, the trial results were not very surprising to me. Stress CMR is a very robust technique that has been around now for over 15 years with a lot of diagnostic and prognostic data supporting its use. Validation of stress CMR-guided management with the prognostically best invasive approach today—invasive FFR-guided management—was what was needed in the evidence base, and MR-INFORM provides that last missing piece.”
Shenoy said the results should change practice, arguing that “stress CMR can and should be used as the first-line test for patients with stable angina and intermediate-to-high risk of coronary artery disease, rather than invasive coronary angiography.”
He pointed out that roughly half of patients in the FFR-guided group did not undergo revascularization. “Thus, stress CMR can safely be used as a gatekeeper to avoid unnecessary invasive coronary angiography,” Shenoy said. “It is a modality that needs to be adopted by more hospitals and performed more frequently.”
Among the strengths of stress CMR, he said, are the lack of radiation and risk of nephrotoxicity and the fact that it can typically be performed in 30 to 45 minutes and interpreted in 10 to 15 minutes. In contrast, he said, CT-derived FFR “takes a few hours.”
Like Douglas, he also pointed to the lower cost associated with stress CMR versus invasive FFR.
“However, if a stress CMR is abnormal, coronary angiography is required before PCI, whereas if invasive FFR is abnormal, they can proceed straight to PCI,” Shenoy said. “Therefore, cost comparisons are complex and we need formal cost-effectiveness analyses, which I am sure will follow publication of the main MR-INFORM paper.”
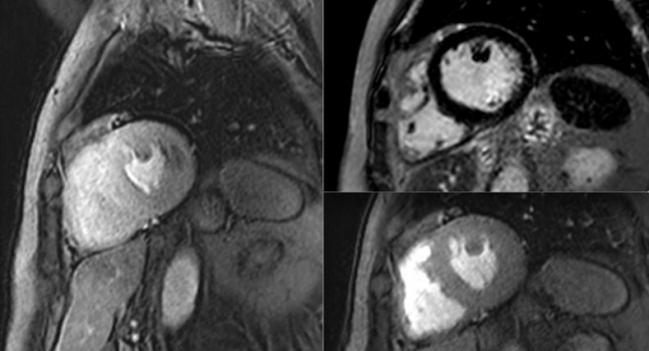
Photo Credit: University Hospital Frankfurt
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Nagel EC. MR-INFORM: stress perfusion imaging to guide the management of patients with stable coronary artery disease. Presented at: ACC 2017. March 17, 2017. Washington, DC.
Disclosures
- MR-INFORM was sponsored by Guy’s and St. Thomas’ Hospital and King’s College London and funded by the Biomedical Research Centre (UK National Institute for Health Research), the German Centre for Cardiovascular Research (DZHK), and Bayer HealthCare.
- Nagel reports receiving consulting fees/honoraria and research grants from Bayer HealthCare and Philips Healthcare, as well as research grants from CVI42 and Medis.
- Douglas reports receiving research funding from GE Healthcare and HeartFlow.
- Shenoy reports no relevant conflicts of interest.


Comments