Complete Revascularization Best for Most ACS Patients With MVD
Cardiogenic shock patients should only undergo culprit-lesion PCI, say experts, and there are limited data on complex lesions.

All patients with acute coronary syndromes, except those who present with or develop cardiogenic shock, should be offered complete revascularization for the treatment of multivessel disease, either before discharge or within the first month after the index procedure, according to a new state-of-the-art paper published this week in EuroIntervention.
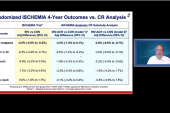
For patients presenting with STEMI and multivessel disease, randomized trials like CVLPRIT, PRAMI, DANAMI-3-PRIMULTI, COMPARE-ACUTE, and—the largest—COMPLETE, along with subsequent meta-analyses, paved the way for complete revascularization. And while the data are relatively weaker in patients presenting with NSTEMI, there is evidence showing that complete revascularization is associated with a lower risk of death and hospital readmission when compared with those who have only the culprit lesion treated.
“The data are more robust in the case of STEMI compared with non-STEMI,” said lead author Valeria Paradies, MD (Maasstad Hospital, Rotterdam, the Netherlands). “For the non-STEMI setting, we have just one randomized trial and the rest of the evidence is from observational registries. But still, we know that in this group of patients, complete revascularization provides a benefit in terms of MACE to the patient. The guidelines recommend going for complete revascularization.”
To TCTMD, Paradies said patients with multivessel disease “represent up to 50% of all acute coronary syndrome patients—it’s quite a large percentage of this population.” Except for those presenting in cardiogenic shock, complete revascularization should be considered in all these individuals, although lesion anatomy and complexity, comorbidities, as well as operator preferences and skills should be taken into account.
Kevin Bainey, MD (Mazankowski Alberta Heart Institute/University of Alberta, Edmonton, Canada), who was not involved in the new review, agreed that complete revascularization should be the approach adopted by operators treating ACS patients with multivessel disease. The COMPLETE trial, for which he was an investigator, was the definitive study in STEMI patients, but Bainey said he also believes the evidence supports complete revascularization in those with NSTEMI. In 2020, for example, he published an observational study showing that complete revascularization was associated with a lower risk of all-cause and cardiovascular death, new MI, and repeat revascularization across a broader group of ACS patients, including those with NSTEMI.
“There’s no big, robust, randomized trials in the non-STEMI patient population, but the general premise to us makes sense,” said Bainey. “We basically showed what COMPLETE showed, including an improvement in survival alone,” he said in reference to their observational analysis of the Alberta COAPT registry.
No Big Trials in NSTEMI
While complete revascularization should be the goal for most patients, it is not recommended for the ACS patient presenting with or developing cardiogenic shock. Here, complete revascularization is to be avoided, given data showing that it is associated with poor clinical outcomes. In the pivotal CULPRIT-SHOCK trial, multivessel PCI in ACS patients with cardiogenic shock was associated with a significantly higher risk of death and severe kidney failure leading to renal-replacement therapy. That trial, said Bainey, was a “game changer,” noting that physicians, based on recommendations from clinical guidelines, would aim for multivessel PCI in patients with cardiogenic shock before the study’s results came to light.
“Now, we try to identify the culprit lesion that brings them in and try to avoid doing anything else,” he said. “The myocardium at that point in time is so fragile. Doing everything in the same setting can potentially be dangerous.”
At present, there are still a number of unknown questions about complete revascularization, said Paradies. For example, it’s not fully known how to best assess the nonculprit lesion or when to intervene. Data from COMPLETE suggest that the timing of revascularization didn’t matter, that the benefits were seen in those treated in the index procedure or several weeks later. However, two ongoing randomized studies—BIOVASC and MULTISTARS AMI—are both comparing an immediate complete revascularization strategy against the staged approach.
In their review, Paradies and colleagues summarize the available evidence on the evaluation of nonculprit lesions, noting that “the optimal time and preferred modality to assess the nonculprit lesions in STEMI patients remains a real diagnostic challenge.” There is evidence supporting the value of physiological assessment of nonculprit lesions in ACS patients with multivessel disease, said Paradies, but she pointed out that the recent FLOWER-MI trial failed to demonstrate the superiority of fractional flow reserve (FFR) over angiographically-guided complete revascularization in STEMI patients presenting with multivessel disease. She noted, however, that event rates in the trial were low and confidence intervals wide around the primary endpoint, making it difficult to translate results of the study to clinical practice.
While the best method of assessing the nonculprit lesions might still be an open question, Bainey pointed out that not only did FLOWER-MI not show a benefit with FFR, but also physiologically-guided PCI is more expensive compared with angiography. “For us, when we saw all that data, it just confirms angiographic-guided, multivessel PCI is the way to go, at least at present,” said Bainey.
Finally, the reviewers summarize the available evidence on complete revascularization of complex lesions in ACS patients, noting that there is no data to recommend PCI of a bystander chronic total occlusion (CTO) in patients with ACS. Nonculprit left-main stenosis is rare in ACS, they say, but if encountered the decision to perform complete revascularization should preferably involve consultation with the heart team.
“It’s a data-free zone,” agreed Bainey, referring on the best approach for ACS patients with CTOs. At their institution, it’s recognized that the risks of revascularizing a CTO are higher, so operators will treat the culprit lesion and then take the patient off the table so that they can be assessed clinically in the outpatient setting. “Once they’ve recovered [from the index PCI], if they are still having ongoing symptoms despite medical therapy, then that would justify for us to proceed with a CTO intervention,” said Bainey. “If they are stable without symptoms and we can’t find another clinical reason to go after the CTO, then we will manage them conservatively, leaving them with incomplete revascularization.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Paradies V, Waldeyer C, LaForgia PL, et al. Complete of revascularization in acute coronary syndrome patients with multivessel disease. EuroIntervention 2021;Epub ahead of print.
Disclosures
- Paradies and Bainey report no conflicts of interest.




Comments