Compression Times Cut With Adjunctive Hemostatic Patch After Transradial Procedures
Use of the patch did not increase the risk of radial occlusion and may help patients be discharged earlier, say operators.
A topical hemostatic patch placed beneath a standard air-bladder bracelet significantly cuts down on the time to hemostasis after transradial procedures without increasing the risk of radial artery occlusion or hematomas, according to a study presented last week.
When using the hemostatic patch (StatSeal; Biolife), the mean time needed to deflate the air-bladder bracelet (TR Band; Terumo) was 66 minutes. By comparison, it was with 113 minutes in patients who received postprocedure compression with the bracelet alone (P < 0.001).
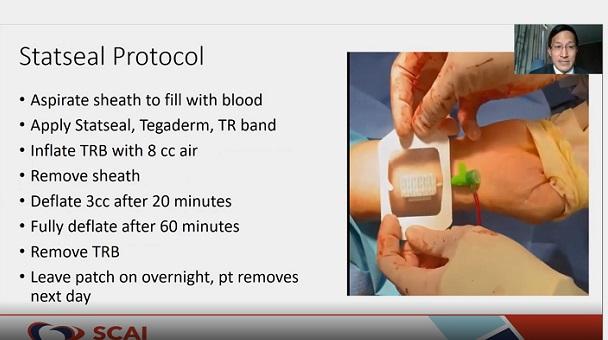
Presenting the study results at the Society for Cardiovascular Angiography and Interventions (SCAI) 2021 Scientific Sessions, Arnold Seto, MD (Long Beach VA Healthcare System, CA), said adjunctive use of the hemostatic patch safely facilitates early deflation of the TR Band after transradial procedures without any of the complications associated with longer or more-aggressive compression, such as radial artery occlusion and hematomas. The patch is composed of a hydrophilic polymer that dehydrates blood and potassium ferrate that clumps the blood solids and proteins together to form a seal at the surface of the skin.
“The potential applications here are that you might have earlier discharge after catheterization, especially after PCI,” said Seto. “You might have reduced nursing burden, time, and costs.” Moreover, the up-front cost of the hemostatic patch is quite affordable, with each priced around $20 to $25, he said.
Senior investigator Jordan Safirstein, MD (Morristown Medical Center, NJ), said that even though the patch itself is “quite cheap,” the decrease in complication rates associated with its use would potentially translate to cost savings on the back end. “You would prevent potential complications that would usually yield additional consults, imaging, and maybe a prolonged hospital stay or an overnight stay,” Safirstein told TCTMD. “By decreasing complications, you would likely save costs.”
The STAT2 Study
Speaking during a SCAI press conference announcing the results, Seto said there is no universal protocol for compression with the TR Band. Shorter compression times lower the risk of radial artery occlusion but are associated with a higher risk of bleeding. Longer compression times, on the other hand, are associated with a higher risk of radial artery occlusion and hematomas. For that reason, the investigators conducted the STAT2 study to determine if a standardized protocol with the hemostatic patch could cut down on the time to hemostasis without increasing the risk of complications.
STAT2 was a multicenter randomized trial of 443 patients undergoing diagnostic catheterization and PCI who received either the hemostatic patch as an adjunct to the TR Band or the TR Band alone. In both treatment arms, the TR Band was deflated after 60 minutes, which is earlier than in most clinical practices, said Seto. The primary endpoint of the trial was the time to successful hemostasis.
Use of the patch with the TR Band cut down on the time to band deflation by about an hour. In the PCI subgroup, the difference was even more pronounced. Here, complete hemostasis occurred after a mean of 68 minutes among those who received the patch and 138 minutes in those who received the TR Band alone (P < 0.001). In patients who received the patch, there was no rebleeding requiring TR Band reinflation. In contrast, the TR Band was reinflated in 67.3% of patients after the 1-hour mark because of continued bleeding.
“It might be a little ooze, it might be a little more than that, but on average you have to reinflate about 2.3 times without the StatSeal,” said Seto.
Instances of any complication—including bleeding requiring intervention, large and small hematomas, and radial artery occlusion—were numerically fewer in the StatSeal arm (4.5% vs 8.6% with the TR Band alone; P = 0.08). In the PCI subgroup, the difference was statistically significant in favor of the hemostatic patch (10.0% vs 24.2%; P = 0.04). Rates of radial artery occlusion were low in the overall cohort, just 0.4% with StatSeal and 0.9% without. Seto noted that 41% of patients in both arms received less than 5,000 units of unfractionated heparin. Their study, he said, suggests that operators may be able to reduce heparin doses for diagnostic procedures when using the hemostatic patch.
Streamlining Procedures
Safirstein said the patch is part of their go-to strategy after transradial PCI.
“Operators who weren’t involved in the study but who witnessed the use of StatSeal and the reproducibility of taking the TR Band off at 60 minutes without much staff involvement, without rebleeding, without hematomas, without radial artery occlusion—it’s become the default strategy in a high-volume cath lab in which we also feature a same-day discharge lounge,” he said. “We hope that it decreases those rare complications that can occur and that it facilitates more-rapid hemostasis and more-rapid discharge.”
Safirstein said they do not typically use the patch in patients who have undergone transfemoral procedures, although they have used it “from time to time” in situations where they have difficulty controlling post-procedure bleeding.
David Cox, MD (Cardiovascular Associates/Brookwood Baptist Hospital, Birmingham, AL), who moderated the session, said that even being able to discharge patients 1 or 2 hours earlier, especially for those who might travel from farther away, can mean the difference between an overnight stay or same-day discharge.
Safirstein agreed, adding that the patch even allows operators to begin cases later in the day. It formalizes the post-PCI hemostasis process, he said, and requires less staffing than the back-and-forth involved with deflating the TR Band to check if the bleeding has stopped.
“It really has made life more streamlined for us,” said Safirstein.
To TCTMD, Seto said several other companies manufacture topical pads or patches to stop bleeding after diagnostic or interventional transradial procedures, among them a catechol conjugated chitosan pad (InnoSEAL; InnoTherapy) and a kaolin-based pad (QuikClot; Z-Medica), both of which were shown to cut the time to hemostasis when compared with pneumatic compression. With the InnoSEAL device, though, rates of radial artery occlusion were quite high at 8.5%, and manual compression for 5 to 10 minutes was still required, he pointed out. Although the InnoSEAL pad was tested as a stand-alone device, not as an adjunct to pneumatic compression, a second study is testing it out when used in conjunction with the TR Band. Seto noted that most of the studies testing these hemostatic devices to date have been small, often with fewer than 100 patients, the exception being the larger InnoSEAL study.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Seto A, Safirstein J, Tehrani D, Schussler J. Radial hemostasis is facilitated with a potassium ferrate hemostatic patch (StatSeal): the randomized controlled Statseal with TR Band assessment trial (STAT2). Presented at: SCAI 2021. April 28, 2021.
Disclosures
- STAT2 was an investigator-initiated, unsponsored clinical trial.
- Seto reports research grants from Philips and Acist and speakers’ bureau fees from Terumo, GE, and Janssen.





Comments