CTO PCI Ups Survival Amid High Levels of Ischemia in Single-Center Series
Another observational study hints that patient selection and perfect technique can yield hard benefits, but RCT proof still lags.

Among patients with heavy baseline ischemic burden treated at an experienced Dutch hospital, PCI for chronic total occlusions (CTOs) was linked with lower rates of all-cause death and nonfatal MI, so long as the patients had no residual ischemia postprocedure.
At experienced centers, CTO PCI practice today is widely accepted for symptom relief, but critics of the protracted, often riskier procedures cite a lack of randomized data showing that the procedure can make a difference in hard outcomes. Notably, though not a CTO study, the ISCHEMIA trial, which was also focused on patients with confirmed ischemia, failed to show that revascularization on top of optimal medical therapy (OMT), versus OMT alone, reduced clinical events, a finding that held true regardless of the level of baseline ischemia.
Investigators for the current study, however, point out that alleviating severe ischemia may be particularly important in the setting of CTOs. “If you have a lot of ischemia at baseline and you're able to reduce that to a minimum or zero, we hypothesized that those patients would do excellent [with CTO PCI] as opposed to those patients who have little ischemia and residual ischemia,” senior author Paul Knaapen, MD, PhD (Vrije Universiteit Amsterdam, Amsterdam, the Netherlands), told TCTMD explaining the rationale of their study, published in the July 12, 2021, issue of JACC: Cardiovascular Interventions.
“It adds to the data, which could not be confirmed in poorly conducted randomized trials, that if you do your job properly in selecting the patients and in doing the technically perfect procedure by reducing the ischemia to nil that those patients actually do have a better outcome,” he said. “It is an observational study, it's not a randomized study, but it is important [in showing] that we need to select the patients better and do a good job with PCI CTO. And that it does seem to have an effect in terms of outcome.”
Commenting on the study for TCTMD, J. Aaron Grantham, MD (University of Missouri Kansas City and Saint Luke's Mid America Heart Institute), noted that questions persist around the true value of common cardiology practices, including both revascularization and stress tests. “This study is yet another to point toward the importance of ischemic-based testing and selecting patients for PCI and for identifying the root causes of any benefit or harm that's caused. And my basic take home message is this is more evidence that CTO PCI can confer benefits to patients. It's probably related to ischemia, but we were not able to confirm that in a randomized trial [ISCHEMIA]. But that was not a CTO trial and it also was a trial with limitations that I think raise reasonable questions. We should persist at attempting to find the truthful answer to these questions.”
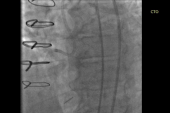
PET Imaging and CTO
For the study, Stefan P. Schumacher, MD (Vrije Universiteit Amsterdam, Amsterdam, the Netherlands), Knaapen, and colleagues evaluated 212 patients (mean age 62 years; 84% male) undergoing CTO PCI at their institution between 2013 and 2019 who prospectively underwent quantitative [15O]H2O PET perfusion imaging before and 3 months after successful procedures.
Notably, 16% of patients were asymptomatic. LV function was preserved in 41% of patients, whereas in LVEF was between 45%-55%, and greater than 45%, in 33% and 26% of patients, respectively. The technical success rate overall was 96%, and complete revascularization was performed in almost all (91%) patients.
After a median follow-up of 2.8 years, the mortality rate was 8%, while 2% experienced a nonfatal MI. Event-free survival was more likely for those with at least three perfusion defect reductions (risk adjusted P = 0.04; HR 0.34; 95% CI 0.13-0.93), as compared with fewer than three. Event-free survival was also better in patients who demonstrated an increase in hyperemic myocardial blood flow (hMBF) above versus below the population median (risk adjusted P < 0.01; HR 0.16; 95% CI 0.05-0.54) after CTO PCI.
Additionally, event-free survival was more likely in patients without any residual perfusion defects after CTO PCI (risk-adjusted P = 0.02; HR 0.22; 95% CI: 0.06-0.76) or with residual hMBF levels of at least 2.3 ml/min/g (risk-adjusted P = 0.03; HR: 0.25; 95% CI 0.07-0.91) at follow-up PET imaging. Also, those with residual hMBF levels above that threshold were more frequently free of angina and dyspnea on exertion at long-term follow-up (P = 0.04).
“To rightfully select patients for revascularization, future studies should put more effort into detection of potential predictors for effective ischemia reduction instead of solely documenting baseline moderate-to-severe ischemia,” the authors write.
Collaterals ‘Insufficient’
In an accompanying editorial, Stéphane Rinfret, MD, SM, and Pratik B. Sandesara, MD (Emory University School of Medicine, Atlanta, GA), detail what they believe are the more notable findings from the study, including the fact that patients with CTOs had on average four perfusion defect segments, with 93% of patients having at least two, as well as all but one patient having hMBF levels below the cutoff value for ischemia. This “[underscores] the fact that virtually all patients with a CTO had inducible ischemia. Such data should question the pertinence of testing for ischemia for single-vessel disease CTO, when symptoms are present, and contractility preserved,” they write. “Altogether, it confirms that collateral channels are insufficient to supply the ischemic CTO territory.”
Grantham agreed. “This shows you that for patients selected for CTO PCI at a high-volume center it does not matter how robust the collaterals are,” he said. “They still have symptoms and so the collaterals are insufficient. And these are data that have been known for a long time. So this notion of a well collateralized CTO should not provide anybody any extra reassurances that collaterals are not sufficient to subtend the myocardium in these patients with CTOs.”
“This is something that the community who does PCI CTO is really looking for,” Knaapen said of the findings. “There are still a lot of noninterventional cardiologists who believe that collaterals are sufficient to prevent ischemia and that patients have no real benefit in terms of outcome if they are being offered PCI of their CTO. [That] is clearly a wrong idea because virtually all patients have ischemia and if you go to a proper site that can conduct PCI CTO in a correct matter—the success rate is very high, complication rate is very low—not only will the patients have benefit in terms of symptom relief but now it also adds improved outcomes.”
He hopes this study will persuade the medical community to refer for CTO PCI more often as the practice is still “being frowned upon” by those who don’t see a benefit. “Withholding these patients treatment based on the philosophy that you cannot change their outcome is probably false.”
Rinfret and Sandesara say the study “adds to the limited data on prognostic benefit of CTO PCI” and the “innovative study design allowed for linking ischemia reduction to long-term outcomes.” However, there remain unanswered questions, they write.
“Although reduction in the number of perfusion defects predicted better outcomes, currently we have no accurate method to predict who will be a ‘good’ versus a ‘poor’ responder to CTO PCI,” according to the editorialists. “Therefore, it is reasonable for the moment to assume that the patient should benefit from an open artery especially in the presence of symptoms and hope that there are no other confounders such as microvascular dysfunction to contribute to residual ischemia. Indeed, the fact that 50% of patients had residual ischemia despite an open artery raises questions on how we currently perform CTO PCI.”
Symptom Relief Remains Key
As for the asymptomatic patients in this study, “it would have been interesting to analyze how ischemia reduction affected outcomes in this subgroup and could have expanded indications of CTO PCI for both symptomatic and asymptomatic patients,” Rinfret and Sandesara write, adding that the primary indication for the procedure should remain symptom relief until more data are available.
That said, prior studies like DECISION-CTO, have shown the immense challenge with recruiting a big enough sample size to show meaningful outcomes in the CTO PCI space. “Therefore, demonstrating the effect of CTO PCI on harder endpoints in RCTs will remain extremely difficult, if not impossible,” they say, adding that the ongoing NOBLE-CTO and ISCHEMIA-CTO trials should give some additional insight.
Grantham said it’s important to question why randomized trials to date have not been able to show an outcome benefit for CTO PCI while observational studies have, especially given the complexity associated with the procedure.
“Is our ability to find this in observational studies simply related to unaccounted for confounding? Or is there something really there that cannot be reproduced in a 400-center trial where the variability in the quality of ischemic testing and the variability in performance of revascularization is tremendous?” he asked. “Those are well described phenomenon that when you cast a net broadly to 400 centers you are going to wind up with some really good places that interpret stress tests well and some places that interpret stress tests less well and perform them less well. And same goes for revascularization, whether it's surgical or percutaneous.”
In Grantham’s experience, he sees “tremendous differences in the quality of the stress test that I'm sent,” he said. “I'll see one report that has a detailed description of the segments involved, the vessel involved, the ischemic burden, the other measures of risk like transischemic dilatation and then I'll see a stress test that just says RCA ischemia.”
This is particularly relevant given that observational studies from multiple experienced centers with “world class” imaging have shown an association of CTO PCI with outcomes, Grantham added.
“One of the key learnings from this is that predicting those who will benefit is important,” he said, noting that CTO PCI in asymptomatic individuals will remain “extremely” controversial. “That's the next phase is figuring out who will benefit and how much they'll benefit if you do ischemia-based revascularization or symptom-based revascularization.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Schumacher SP, Stuijfzand WJ, de Winter RW, et al. Ischemic burden reduction and long-term clinical outcomes after chronic total occlusion percutaneous coronary intervention. J Am Coll Cardiol Interv. 2021;14:1407-1418.
Rinfret S, Sandesara PB. Reducing ischemia with CTO PCI: good news, but questions remain. J Am Coll Cardiol Interv. 2021;14:1419-1422.
Disclosures
- Schumacher, Knaapen, and Sandesara report no relevant conflicts of interest.
- Rinfret reports serving as a consultant for Boston Scientific, Teleflex, Medtronic, Abbott, and Abiomed.
- Grantham reports receiving honoraria and speaking fees from Boston Scientific, Abbott Vascular, and Asahi Intecc; institutional research funding from Boston scientific to support the OPEN CTO trial; and serving on the advisory boards of Boston Scientific and Abbott Vascular.




Comments