Fixed-Dose Combo Therapy Slashes CVD Risk in Primary Prevention
When aspirin was added, a meta-analysis saw no increase in bleeding but gained an incremental reduction in CVD risk.

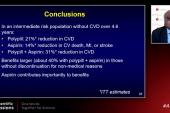
Use of fixed-dose combination therapy, including a polypill, significantly cuts the risk of a first major cardiovascular event in people without preexisting disease, according a new meta-analysis.
Combining TIPS-3 and PolyIran, both of which used a polypill, along with HOPE-3, a study that randomized patients to fixed-dose combination therapy, investigators observed a 38% lower relative risk of cardiovascular death, MI, stroke, or arterial revascularization over 5 years of follow-up when compared placebo or usual care (HR 0.62; 95% CI 0.53-0.73). The relative reduction in risk was more pronounced when aspirin was included as part of treatment, researchers report, and didn’t come at an increased cost of bleeding.
For lead investigator Philip Joseph, MD (Hamilton Health Sciences/Population Health Research Institute, Hamilton, Canada), the findings confirm that use of multiple agents, either as part of a fixed-dose combination strategy or in a single pill, can have a significant impact on the risk of ischemic events in primary prevention.
“The effects on fatal and nonfatal cardiovascular events are pretty impressive when you use these combinations—a statin, at least two blood pressure-lowering pills, and then plus or minus aspirin,” Joseph told TCTMD. “With or without aspirin, there are large effects, but obviously the benefit is bigger when you include it.”
We’ll never be able to wipe out cardiovascular disease unless we prevent the first event. Salim Yusuf
Senior investigator Salim Yusuf, MBBS, DPhil (Hamilton Health Sciences/Population Health Research Institute), a longtime proponent of the polypill concept, said the new meta-analysis provides a better estimate of the intervention’s effect size than any of the smaller studies could provide alone. With respect to aspirin, Yusuf said it provides an incremental benefit when combined with a fixed-dose strategy, one that leads to a pretty substantial overall gain in terms of relative risk reduction. Both he and Joseph were investigators for the TIPS-3 and HOPE-3 trials.
“When put together with the other drugs, it’s a huge benefit,” Yusuf told TCTMD. “We saw a 50% reduction in cardiovascular disease. In primary prevention, that’s really big, and the reason is that 80% of cardiovascular disease originates in people who have never had a heart attack or stroke before. The focus on secondary prevention makes a lot of sense, but it’s inadequate. We’ll never be able to wipe out cardiovascular disease unless we prevent the first event. This shows there is a way of doing that at low cost and doing it safely.”
A 32% to 47% Reduction in Major CVD
The new meta-analysis, which was presented during a Late-Breaking Science session at the European Society of Cardiology (ESC) Congress 2021 and published simultaneously in the Lancet, included 18,162 participants from the three studies. The mean age of the population was 63 years, and 50% were women. Roughly two-thirds of participants had hypertension, one in five had diabetes, and nearly one-quarter were smokers. Patients were considered at intermediate risk for cardiovascular disease, with an estimated 10-year risk of 17.7%.
In TIPS-3, the intervention included a daily oral polypill that consisted of simvastatin 40 mg, ramipril 10 mg, atenolol 100 mg, hydrochlorothiazide (HCTZ) 25 mg, and aspirin 75 mg. In PolyIran, the polypill consisted of atorvastatin 20 mg, HCTZ 12.5 mg, enalapril 5 mg (or valsartan 40 mg), and aspirin 81 mg. HOPE-3, which used a fixed-dose combination strategy instead of a single polypill, included patients treated with rosuvastatin 10 mg, candesartan 16 mg, and HCTZ 12.5 mg.
The effects on fatal and nonfatal cardiovascular events are pretty impressive when you use these combinations. Philip Joseph
In the overall population, which included patients treated with and without aspirin, the intervention led to a significant 1.9% absolute reduction in risk of the primary endpoint. Additionally, treatment reduced the individual components of the primary endpoint, including cardiovascular death (1.6% vs 2.5%; P < 0.0001), MI (0.8% vs 1.5%; P < 0.0001), stroke (0.6% vs 0.9%; P = 0.0002), and revascularization (0.4% vs 0.8%; P = 0.002).
In the analysis of patients who received aspirin as part of the combination, treatment led to an even larger absolute reduction in the risk of the primary endpoint (2.6% with fixed-dose combination vs 4.8% with control; P < 0.0001). Here again, there were significant reductions in the risk of cardiovascular death, MI, and stroke, although the difference in the risk of revascularization was not significant. In the analysis excluding patients who received aspirin, the fixed-dose combination strategy also reduced the risk of the primary endpoint (3.3% vs 4.9%; P < 0.0001), as well as significantly reduced all individual components of the primary endpoint.
Mahmoud Al Rifai, MD (Baylor College of Medicine, Houston, TX), who wasn’t involved in the meta-analysis, said the reduction in major CVD events lines up with that observed in the individual trials. Primary and secondary prevention involve “a multifaceted approach,” he stressed. “There are different risk factors, and all need to be well controlled to prevent cardiovascular disease. The more pathways you target, the more risk reduction you’re going to see.”
To TCTMD, Al Rifai called the polypill a “beautiful concept,” highlighting the difficulties physicians can have with patients adhering to their medications. “Having one pill that can treat blood pressure and cholesterol, plus or minus aspirin, is a very attractive strategy to improve adherence, especially in patients who might be at high risk,” he said. “Those high-risk patients need to have all their risk factors controlled and having just one pill that treats them simultaneously is a very good choice, and I think it is future going forward.”
The polypill itself, he said, isn’t quite perfected yet in terms of what’s in it, and at what doses, but he suspects that can be addressed with multiple formulations in the future. “I’m a big fan of the polypill, but I do think more research needs to be done before it becomes mainstream,” said Al Rifai.
During the ESC presentation, Joseph noted the trials included patients from high-, middle-, and low-income countries so the results are applicable globally. By their estimates, the fixed-dose combination strategy could prevent 5 to 10 million CVD events each year and go a long way toward the United Nations’ goal of reducing premature deaths from noncommunicable diseases by one-third by 2030.
Aspirin: Risks and Benefits
To TCTMD, Joseph said there is a lot of discussion over the use of aspirin in primary prevention. The American College of Cardiology/American Heart Association guidelines for CVD primary prevention recommend against its broad use based on several clinical trials—ASPREE, ARRIVE, and ASCEND—that showed the balance of benefit versus risk doesn’t favor its use.
“The aspirin controversy in primary prevention is interesting,” said Joseph. “When we look at meta-analyses and the more recent trials, they do show there is a reduction in MI, stroke, and revascularization. Overall, there’s probably about an 11% reduction in total ischemic CVD events, and slightly larger reductions in some of the individual outcomes. Aspirin does reduce ischemic events, but the controversy relates to the balance of bleeding. It’s a good question—is the reduction in ischemic events comparable to the increased risk of bleeding? When we talk about really significant bleeding events, like hemorrhagic stroke or major GI bleeding or a fatal bleeding, those aren’t very common.”
The meta-analysis, said Joseph, shows that if clinicians are looking to maximize the reduction in risk, then that combination strategy includes aspirin. In their analysis, the number needed to treat (NNT) to prevent one primary outcome event in the overall population was 52; in those who received aspirin, the NNT was 37. With bleeding, Joseph said they observed less compared with other trials, and while the number of GI bleeds was numerically higher in the aspirin-treated patients, the difference wasn’t significant. There were no significant differences in hemorrhagic stroke or death due to bleeding either.
If their calcium score is more than a 100, I would be inclined to prescribe aspirin. Mahmoud Al Rifai
“It seems like the strategy—if the goal is to maximize cardiovascular risk reduction at the population level—the three agents should be considered together,” said Joseph, referring to statins, antihypertensive agents, and aspirin. “The safety and tolerability are pretty reasonable based on our analysis.”
Joseph added that their results should be taken in context with results from other trials.
To TCTMD, Yusuf said that one of the problems with aspirin for primary prevention is that physicians have historically considered its use as a single agent rather than as part of a package with statins and antihypertensive drugs making up the polypill or a fixed-dose combination strategy. Like Joseph, he noted they observed no excess bleeding with the addition of aspirin, which might be the result of the patients studied or the possible reduction in blood pressure, which would in turn lower the risk of hemorrhagic stroke. “It could be multiple factors,” he said. “It could be that in the types of people we studied things just worked out.”
Al Rifai said aspirin is “one of those tough medicines,” noting that he typically doesn’t use it for primary prevention, particularly if the patient might be at risk for bleeding. The issue is trickier in younger-to-middle-aged adults (40 to 70 years) who aren’t at a high risk for bleeding, though. Still, his general tendency is not to prescribe aspirin here either, unless there are other factors that might change his mind.
“If their calcium score is more than a 100, I would be inclined to prescribe aspirin,” said Al Rifai. “A score more than 100 has been shown in prior studies to result in event rates similar to a secondary-prevention population. That’s a particularly higher-risk group that might benefit, but every time you prescribe a medicine there is going to be a risk and benefit.” Additionally, he might be inclined to prescribe aspirin in a patient with an estimated 10-year risk of CVD exceeding 20%.
Global Applications
In terms of the big picture, Yusuf imagines the polypill being useful to a broad swath of the population.
“I think it’s going to be applicable everywhere. There’s substantial undertreatment, even in rich countries like Canada. The polypill will help us improve primary prevention. You might start with the higher-risk people, like those with hypertension, diabetes, high cholesterol, obesity, or smokers, but once you do that, that’s 80% of the general population over the age of 50. Take the people over age 50, and either give everybody the polypill, which a lot of people react to, or just to those with a risk factor. But with 50% [of the population] with hypertension, 10% with diabetes, and another 10% or 15% with other conditions, pretty soon you’re at 80% of the population.”
Yusuf also emphasized that the benefit of the fixed-dose combination strategy was seen across all subgroups—men and women, those with and without hypertension, those with and without diabetes, and across a range of ages, baseline LDL-cholesterol levels, systolic blood pressure, and risk. “There was no group we found that didn’t have a benefit,” said Yusuf.
In an editorial, Jonathan Mant, MBBS, MD (University of Cambridge, England), and Richard McManus, MBBS, PhD (University of Oxford, England), say that pharmacotherapy needs to be as simple as possible for people to take it. “Although a polypill strategy might sit uncomfortably with precision medicine, there is now a substantial evidence base that such an approach is effective at reducing cardiovascular disease,” they write. “Guideline writers and policy makers should consider how to incorporate this evidence base into guidelines and policies.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Source(s): Joseph P, Roshandel G, Gao P, et al. Fixed-dose combination therapies with and without aspirin for primary prevention of cardiovascular disease: an individual participant data meta-analysis. Lancet. 2021;Epub ahead of print.
Disclosures
- Yusuf reports grants from the Canadian Institutes of Health Research, Wellcome Trust, AstraZeneca, and Cadila Pharmaceuticals related to conducting the HOPE-3 or TIPS-3 studies. He reports receiving honoraria and reimbursement for travel expenses from AstraZeneca, Bayer, Boehringer Ingelheim, and Ferrer.
- Joseph reports grant support from the Institutes of Health Research, Heart and Stroke Foundation of Ontario, Cadila Pharmaceuticals, and AstraZeneca related to the TIPS-3 or HOPE-3 studies.




Comments