Full AEGIS-II Results: Raising HDL With Apo A-I No Help After Acute MI
So is this the end for the HDL-raising hypothesis? Maybe, maybe not, experts argue after seeing the full results.
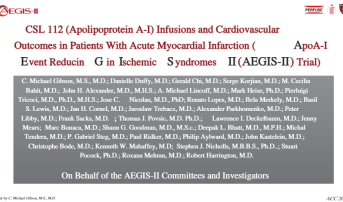
ATLANTA, GA—Full results of the phase III AEGIS-II trial, presented today at the American College of Cardiology 2024 Scientific Session, show that the investigational cholesterol efflux enhancer CSL112 does not reduce MACE at 90, 180, or 365 days after acute MI compared with placebo.
However, exploratory analyses seem to indicate raising HDL cholesterol in certain subgroups may have a beneficial effect.
Cardiologists have long hoped that raising HDL cholesterol might improve cardiovascular outcomes after acute MI. CSL112 (CSL Behring) was developed using human plasma-derived apolipoprotein A-I, the primary functional component of high-density lipoproteins, with the aim of increasing cholesterol efflux to improve CV outcomes.
The neutral primary results from AEGIS-II call into question whether the HDL-raising hypothesis is still relevant.
C. Michael Gibson, MD (Baim Institute for Clinical Research, Harvard Medical School, Boston, MA), who presented the findings today in a late-breaking clinical trial session said that depends on the patient. “I would say 35 out of 35 steering committee members think that the reduction in MI, the reduction in cardiovascular death and MI, seems to give us a signal that is consistent with the role of HDL in stabilizing plaque,” he told TCTMD. “Stroke didn’t benefit, but there’s a lot of reasons you have stroke. The majority of us think the HDL hypothesis is still alive and kicking, but you need to be hyperlipidemic.”
AEGIS-II was simultaneously published in the New England Journal of Medicine. Ninety-day outcomes were previously released as top-line results in February, as reported by TCTMD.
The majority of us think the HDL hypothesis is still alive and kicking, but you need to be hyperlipidemic. C. Michael Gibson
Early success with intravenous CSL112 showed its ability to successfully increase cholesterol efflux capacity in healthy subjects as well as its safety and tolerability in patients with ACS. The AEGIS-II trial was previously referred to as the “last big shot on goal for HDL cholesterol.”
In a press conference, Pamela Morris, MD (The University of South Carolina, Charleston), said she, and likely many others, “let out a great sigh of disappointment with the release of these results.”
AEGIS-II Findings
For the study, Gibson and colleagues randomized 18,219 patients (mean age 65 years; 74% male) following acute MI (50.5% STEMI) to receive either four weekly 6-g infusions of CSL112 or matching placebo, with the first infusion given within 5 days after first medical contact. Baseline median LDL- and HDL-cholesterol levels were 84 and 39 mg/dL, respectively.
At 90 days, there was no significant difference between the study and placebo groups in the risk of the primary composite endpoint of MI, stroke, or cardiovascular death (4.8% vs 5.2%; HR 0.93; 95% CI 0.81-1.05). Similarly, no differences were observed at 180 days (6.9% vs 7.6%; HR 0.91; 95% CI 0.81-1.01) or 365 days (9.8% vs 10.5%; HR 0.93; 95% CI 0.85-1.02).
There were no differences in any of the key prespecified secondary endpoints, with the exception of MI, which was less common in the study arm versus placebo population at both 180 days (5.0% vs 5.7%; HR 0.87; 95% CI 0.77-0.99) and 365 days (7.2% vs 7.9%; HR 0.90; 95% CI 0.81-1.00).
Broken down in an exploratory analysis that was simultaneously published in the Journal of the American College of Cardiology, Thomas Povsic, MD, PhD (Duke Clinical Research Institute, Durham, NC), and colleagues showed numerically lower rates of type 1 MI at 90 days (1.4% vs 1.7%), 180 days (2.2% vs 2.6%), and 365 days (3.4% vs 3.9%) with CSL112 compared with placebo infusions. The same was seen for type 4b MI at 90 days (0.5% vs 0.8%), 180 days (0.6% vs 0.9%), and 365 days (0.8% vs 1.0%).
Adverse and hypersensitivity event rates were similar between the study groups, but there were significantly more immune system disorder events leading to discontinuation in the CSL112 cohort (14 vs 4; P = 0.02). Renal safety was good for the investigational agent with fewer acute kidney injury events in this group compared with placebo (6.3% vs 7.2%; P = 0.02).
The findings were maintained in a variety of subgroups. However, an exploratory analysis hinted at greater benefit with CSL112 infusions for patients with baseline hyperlipidemia (LDL cholesterol ≥ 100 mg/dL). This group saw significantly lower rates of the primary composite endpoint compared with those receiving placebo at 90 days (3.4% vs 4.9%; HR 0.69; 95% CI 0.53-0.90), 180 days (5.3% vs 7.3%; HR 0.71; 95% CI 0.57-0.88), and 365 days (7.8% vs 9.9%; HR 0.78; 95% CI 0.65-0.93). This group also saw significant benefits for the individual outcomes of CV death, MI, and CV death/MI. For patients with baseline LDL cholesterol < 100 mg/dL, the event curves were almost transposable.
Future Efforts?
In an accompanying editorial, Christie M. Ballantyne, MD, and Vijay Nambi, MD, PhD (both from Baylor College of Medicine, Houston, TX), argue that enough open questions remain to warrant future work in this space, including the effect of baseline cholesterol efflux capacity values on outcomes, the potential for longer-term clinical effects of drugs like CSL112, and the feasibility of long-term weekly infusions.
“Before declaring that the AEGIS-II trial is the final curtain call and retiring therapies aimed at the ‘Highly Disappointing Lipoprotein,’ perhaps a reconceptualization is needed that focuses on developing better assays for characterizing HDL functions that can be used in conjunction with genomics, metabolomics, proteomics, and transcriptomics to identify new targets and the correct population in which to test therapies to improve cholesterol efflux and the functionality of HDL,” they write.
Until that can happen, Ballantyne and Nambi suggest “it is time to shelve HDL therapeutics and put them on the ‘injured reserve list’ of preventive therapies for cardiovascular disease.”
Asked whether she thought there should be much more effort expended in the HDL-raising space, Morris hedged her bets. “The answer is, I don't know,” she said. “In part because we really thought there was an association on a broad epidemiological basis that higher HDL is better. We also know that too high HDL is not good, especially if it's too high because of alcohol or something else. So there's a sweet spot for raising HDL cholesterol. But we've done that a variety of ways and it doesn't work.”
Instead, she suggested, maybe more emphasis should be placed on lowering LDL cholesterol given the wide swath of agents now available, including nonstatins. “I would have liked to have seen the patient population with extremely well treated LDL and then see what the additional benefit might be,” Morris said. “I think when you take a therapy designed to get at residual risk and you haven't controlled the easy stuff first, then you've kind of got to wonder what you're doing.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Gibson CM, Duffy D, Korjian S, et al. Apolipoprotein A1 infusions and cardiovascular outcomes after acute myocardial infarction. N Engl J Med. 2024;Epub ahead of print.
Ballantyne CM, Nambi V. HDL therapeutics — time for a curtain call or time to reconceptualize? N Engl J Med. 2024;Epub ahead of print.
Povsic TJ, Korjian S, Bahit C, et al. Effect of CSL112 on recurrent myocardial infarction and cardiovascular death: insights from the AEGIS-II trial. J Am Coll Cardiol. 2024;Epub ahead of print.
Disclosures
- The study was supported by CSL Behring.
- Ballantyne reports serving as a consultant to Alynlam Pharmaceuticals, Amgen, AstraZeneca, Merck, Novartis, Novo Nordisk, Pfizer, Regeneron, and Roche Diagnostics Corporation.
- Nambi reports holding stock in Abbott Laboratories and Insera Therapeutics as well as receiving a grant/contract from Amgen.





Comments