Full AGENT IDE Results Affirm Benefits of DCB for In-Stent Restenosis
(UPDATED) The device represents a huge advance, but not a panacea, for clinicians dealing with a common issue, says Ajay Kirtane.
WASHINGTON, DC—-Results from the full cohort of patients treated with a newly approved DCB for in-stent restenosis confirm its superiority over an uncoated balloon, and investigators say it will prevent having to put in more layers of metal stents to tackle a common problem.
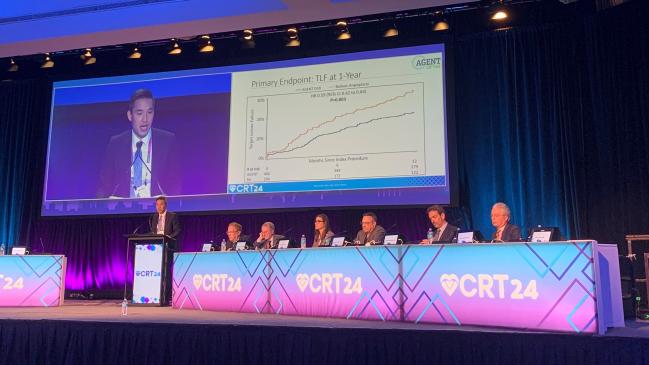
“More than 40% of patients presented with restenosis of multiple layers of stent, representing a truly high-risk population and a population for which clinicians would be uncomfortable typically implanting yet another stent,” AGENT IDE principal investigator Robert Yeh, MD (Beth Israel Deaconess Medical Center, Boston, MA), said in presenting the data here at CRT 2024.
Earlier this month, the Agent (Boston Scientific) became the first coronary DCB in the United States to be approved for the treatment of in-stent restenosis (ISR). It had been granted breakthrough device designation by the US Food and Drug Administration in 2021 based on unmet clinical need, and was already available in Europe, parts of Asia Pacific, and Latin America for the treatment of ISR and previously untreated small-vessel coronary disease.
“We see a lot of these patients, and many have to go for bypass surgery, many are told they have no options,” AGENT IDE study chair Ajay Kirtane, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), told TCTMD.
Late last year, the AGENT IDE investigators reported an interim analysis of the first 480 randomized patients showing less TLF at 12 months with the DCB versus an uncoated balloon, with the difference being driven by a relative halving of the risks of TLR and target-vessel MI. The AGENT IDE results were published simultaneously in JAMA and include the full 600-patient cohort, 406 of whom received the DCB.
Those treated with the Agent DCB had 1-year rates of TLF—the composite of ischemia-driven TLR, target vessel-related MI, or cardiac death—of 17.9% compared with 28.6% for the uncoated balloon group, meeting the criteria for superiority (HR 0.59; 95% CI 0.42-0.84). Follow-up is planned through 5 years.
“These were patients who were treated aggressively in the procedure to make sure that all the stent dimensions and everything else was prepared very well and then finished with the drug-coated balloon,” Kirtane noted.
Full Cohort Results
For the study, Yeh, Kirtane and colleagues analyzed the 600 randomized patients (mean age 68 years; 26% female; 7% Black) who had 1-year clinical follow-up or death. There were high rates of diabetes (51%), multivessel CAD (79%), and prior CABG (30%). In 43% of patients, multiple prior stents were present at the site of the target lesion.
Patients had ISR of a lesion previously treated with BMS or DES that was less than 26 mm in length and between 2.0 and 4.0 mm in reference vessel diameter. Symptomatic patients were enrolled if they had target lesion stenosis < 100% but greater than 50%, and asymptomatic patients were enrolled if they had target lesion stenosis greater than 70%.
Conventional angioplasty techniques were used in all patients prior to randomization to the low-dose paclitaxel-coated DCB or uncoated balloon. Intravascular imaging was used in 74%.
Procedural success was 92.1% in the DCB group and 88.7% in the uncoated balloon group (P = 0.17), and technical success rates were 93.4% and 89.7%, respectively (P = 0.12).
Compared with the uncoated balloon group, TLR was less frequent in the DCB group (13.0% vs 24.7%; HR 0.50; 95% CI 0.34-0.74), as was target vessel-related MI (5.8% vs 11.1%; HR 0.51; 95% CI 0.28-0.92). The incidence of cardiac death was similar in both groups.
Definite or probable stent thrombosis was more common in the uncoated balloon group, occurring in six patients compared with none in the DCB group at 1 year.
In prespecified subgroup analyses, the rate of TLF was lower in the DCB group than in the uncoated balloon group in those with multilayer ISR (23.8% vs 40.0%; HR 0.55; 95% CI 0.34-0.87) and in those with diabetes (21.6% vs 29.2%; HR 0.71; 95% CI 0.43-1.17).
According to the study investigators, DCB may be particularly useful in the multilayer ISR patients “where additional stenting would result in three or more layers of stent that may further reduce lumen area and limit future therapeutic options by further constraining the vessel wall,” they write.
“My take-home is that this is a huge advance, but it's not a panacea,” Kirtane told TCTMD. “You still have to be a clinical physician to figure out what the best therapy is for an individual patient.”
Still a Role for DES
Following Yeh’s presentation here, co-moderator Antonio Colombo, MD (Humanitas IRCCS, Milan, Italy), said the data are clear that POBA should not be used in ISR and echoed Kirtane’s advice about the importance of optimizing the vessel prior to DCB use and choosing the best interventional tool.
“Some types of in-stent restenosis such as diffuse [or] proliferative will not respond well to DCB. We almost never use only DCB in those lesions,” he said. Colombo also said while multiple stent layers are not ideal, there are scenarios when another stent may be warranted, rather than opting for a DCB.
Panelist J. Dawn Abbott, MD (Brown University, Providence, RI), said the availability of a DCB for ISR comes as a relief for many US operators who had lists of patients they would have liked to enroll in AGENT IDE. However, she said some practical factors will be in play as the device hits the market.
“One big factor in the United States will be that the Agent device is going to be priced at a breakthrough technology cost, which is going to be very expensive” she said. “We're going to have to decide how these are brought in and utilized.”
At a price estimated to be 10-fold more expensive than a DES, patients with ISR who are suitable for treatment with a DES will probably still get that as the treatment of choice, she added.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Yeh RW, Shlofmitz R, Moses J, et al. Paclitaxel-coated balloon vs uncoated balloon for coronary in-stent restenosis: the AGENT IDE randomized clinical trial. JAMA. 2024;Epub ahead of print.
Disclosures
- Kirtane reports institutional funding (including research grants and fees for consulting and/or speaking) to Columbia University and/or the Cardiovascular Research Foundation from Medtronic, Boston Scientific, Abbott Vascular, Abiomed, CSI, CathWorks, Siemens, Philips, and Recor Medical; consulting fees from Neurotronic; and travel expenses/meals from Medtronic, Boston Scientific, Abbott Vascular, Abiomed, CSI, CathWorks, Siemens, Philips, Recor Medical, Chiesi, Opsens, Zoll, and Regeneron.
- Yeh reports receiving grants/research support from Abbott Vascular, BD Bard, Boston Scientific, Cook Medical, Philips Medical, and Medtronic, and consulting for Abbott Vascular, Boston Scientific, CathWorks, Elixir Medical, Infraredx, Medtronic, Shockwave Medical, and Zoll.




Comments