German COVID-19 Autopsy Data Show Thromboembolism, ‘Heavy’ Lungs
The data support the idea that some patients may need anticoagulation to prevent pulmonary embolism.
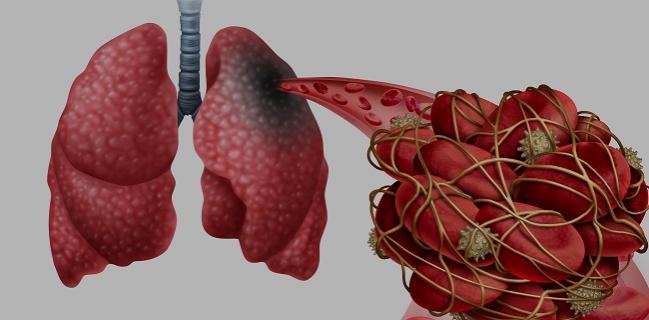
Autopsy data from Germany on a dozen patients who died from COVID-19 confirm that thromboembolic events are common and may be unsuspected at the time of death.
“The high rate of death-causing pulmonary embolism at autopsy correlates well with the unsuccessful resuscitation of three of four patients, two of whom died out of the hospital,” write Dominic Wichmann, MD (University Medical Center Hamburg-Eppendorf, Germany), and colleagues. “Apart from that, no preclinical evidence had been reported of pulmonary embolism or deep venous thrombosis.”

Commenting on the study for TCTMD, Behnood Bikdeli, MD (NewYork-Presbyterian Hospital/Columbia University Irving Medical Center, New York, NY, and Yale Center for Outcomes Research & Evaluation, New Haven, CT), urged caution in interpreting and generalizing such a small autopsy study. He noted that interest in COVID-19 has resulted in studies that are much smaller and less comprehensive than they might ordinarily be in a non-pandemic situation, but that “are deserving of publication and dissemination” due to the need to gather data quickly.
“The take-home message from my end is that it reflects what we've observed in a series of smaller clinical studies, that thrombosis is an important and fairly common phenomenon in patients with COVID-19,” Bikdeli said. In a recent review paper in the Journal of the American College of Cardiology, he and his colleagues summarized what is known about venous thromboembolism in COVID-19 patients and issues surrounding therapeutic anticoagulation, including potential interactions with COVID-19 therapies.
Lungs More Than Twice Normal Weight
The autopsy study by Wichmann and colleagues, published online May 6, 2020, ahead of print in Annals of Internal Medicine, was possible because Hamburg, Germany, ordered mandatory autopsies for all patients who died with confirmed COVID-19. The autopsies included full-body CT, histology, and virology, with an average interval from death to postmortem imaging and autopsy of 1 to 5 days. The median age of the 12 patients was 73 years and all had at least one pre-existing chronic medical condition identified, including obesity, CAD, asthma or chronic obstructive pulmonary disease, PAD, diabetes, or neurodegenerative diseases.
In every case, the lungs or pulmonary vascular system were identified as the cause of death. Wichmann et al describe the lungs of these patients as “congested and heavy.” While a standard combined lung weight at death averages 840 g for men and 639 g for women, the COVID-19 patients had mean combined lung weights of 1,988 g, with one 85-year-old man having a lung weight more than four times the male average at 3,420 g.
Massive pulmonary embolism arising from thrombi located in the deep veins of the lower extremities was the cause of death in four of 12 cases. In three others, fresh deep venous thrombosis was present in the absence of pulmonary embolism. Additionally, the investigators also found fresh thrombosis in the prostatic venous plexus of six of nine men.
Other findings included elevated levels of lactate dehydrogenase, D-dimer, and C-reactive protein. In four of 10 patients, mild thrombocytopenia was present. Procalcitonin immunoassays were mostly negative except in one patient with pneumonia.
Wichmann and colleagues say the small data set is important since only three case reports have been published on complete autopsies in patients with COVID-19.
To TCTMD, Bikdeli said the data help dispel the idea that all COVID-19 deaths are clear-cut acute respiratory distress syndrome (ARDS).
“To some extent, this is in line with studies from decades ago showing that almost half of venous thromboembolic events, if not more, are not being recognized prior to death,” he observed. “It reinforces the suspicion that thrombotic events are an important feature of this disease. It's not just the pulmonary syndrome. It's a multiorgan dysfunction syndrome, which is in part manifest by disease of the blood vessels and venous and arterial thrombotic events.”
In light of the need for caution, Bikdeli said not only is the study small, it is also from a single center and is subject to inherent selection bias in terms of who underwent autopsy and who did not. Nevertheless, he was in agreement with the authors’ conclusions, adding that “robust evidence for patient management is still scant and we need additional prospective studies both to better understand the exact point estimates of how frequent these events are and also to find treatment strategies that can safely mitigate patient outcomes.”
How, Who, and When to Anticoagulate
According to Wichmann and colleagues, the elevated D-dimer levels, a sign of coagulopathy, may help identify patients who could benefit from anticoagulant therapy.
The critical issue is how do we diagnose them, how do we mitigate them before they happen, and how do we manage them most effectively. Behnood Bikdeli
At the moment, one of the most pressing, clinically relevant questions at hand is understanding the anticoagulation theory, including who needs it when they have COVID-19 and when in the disease course they should get it, Bikdeli said. His group and others have embarked on randomized trials, and an upcoming consensus document will delve into anticoagulation research priorities for various COVID-19 patient populations, including: those with COVID-19 who are not ill enough to be hospitalized but potentially immobile enough to need preventive therapy, those hospitalized but not ill enough for the ICU, those in the ICU but not on a ventilator, and those on ventilator support.
Bikdeli said a consensus document is needed because “right now everyone is sort of doing their own thing,” which leads to mixed signals for clinicians who might be willing to try regimens that seem reasonable but have little data to back them.
Finally, Bikdeli said it is both “possible and concerning” that unrecognized thromboembolic events are responsible for situations where COVID-19 patients appear to be recovering and then decline rapidly and die.
“I have witnessed many thrombotic events in these patients, and their rates are above and beyond anything that I, for one, have ever seen before,” he added. “For sure, there is something going on there and we have hypotheses about why it is happening. The critical issue is how do we diagnose them, how do we mitigate them before they happen, and how do we manage them most effectively.”
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Wichmann D, Sperhake J-P, Lütgehetmann M, et al. Autopsy findings and venous thromboembolism in patients with COVID-19: a prospective cohort study. Ann Intern Med. 2020;Epub ahead of print.
Disclosures
- Wichmann reports no relevant conflicts of interest.
- Bikdeli reports serving as a consulting expert on behalf of plaintiffs for litigation related to a specific type of inferior vena cava filters.


Comments