Good TAVI Results Seen in Bicuspid Aortic Stenosis: TVT Registry
Careful patient selection is key to ensure outcomes comparable to what surgery can achieve, experts say.
In patients with bicuspid aortic stenosis who are at low surgical risk, TAVI with a contemporary balloon-expandable valve provides outcomes similar to those achieved in patients who have tricuspid aortic valves, according to data from the Society of Thoracic Surgeons/American College of Cardiology (STS/ACC) TVT Registry.
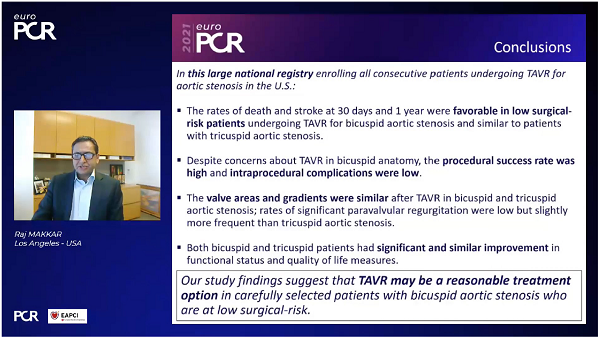
“Despite concerns about TAVR in bicuspid anatomy, the procedural success rate was high and intraprocedural complications were low,” Raj Makkar, MD (Smidt Heart Institute at Cedars-Sinai, Los Angeles, CA), reported during the virtual EuroPCR 2021.
Moreover, stroke and death rates were “favorable” in patients with bicuspid valves and were not significantly different in the hospital, at 30 days, or at 1 year from rates observed in patients with tricuspid valves, he said. The two groups also derived similar benefits in terms of valve areas and gradients, functional status, and quality of life.
“Our study findings suggest that TAVR may be a reasonable treatment option in carefully selected patients with bicuspid aortic stenosis who are at low surgical risk,” Makkar concluded.
Commenting for TCTMD, Mohamed Abdel-Wahab, MD (Leipzig Heart Center, Germany), said the results are encouraging, but stressed the importance of careful patient selection.
“With the data that are accumulating now, we are starting to understand which patients we should treat, which patients we shouldn’t be treating,” he told TCTMD. “This study reinforces the fact that when we pay good attention to patient selection, we can achieve outcomes that are almost as good as what we do for tricuspid patients, which really moves the field forward.”
Though randomized trials focused on these specific patients are still required, “bicuspids should not be considered taboo anymore for catheter-based replacement,” Abdel-Wahab said. “On the other hand, they should still be recognized as a special population.”
Filling an Evidence Gap
Though TAVI is now approved for use in patients with low surgical risk, the pivotal trials supporting that indication excluded patients with bicuspid aortic stenosis out of concerns about how the devices would perform in that group, Makkar told TCTMD. That was a reasonable decision at the time, he said, “but if you are going to encounter more bicuspid patients in clinical practice now, I think it is reasonable that we accumulate data in a systematic fashion in these patients.” According to some estimates, he noted, bicuspid valves are found in about half of patients with aortic stenosis who are young and have low surgical risk.
Bicuspids should not be considered taboo anymore for catheter-based replacement. Mohamed Abdel-Wahab
For this study, Makkar and his colleagues examined data from the STS/ACC TVT Registry on 159,661 patients undergoing TAVI with the Sapien 3 or Sapien 3 Ultra valve (Edwards Lifesciences) between June 2015 and October 2020; 4.4% of patients had bicuspid aortic stenosis. The investigators focused on the subset with low surgical risk (STS score < 3%), comparing outcomes of 3,168 patients with bicuspid valves with those of an equal number of patients with tricuspid aortic valves after propensity matching. Mean patient age was 69, and 70% were men. Average STS score was 1.7%.
There were some procedural differences between the bicuspid and tricuspid groups. Although the vast majority in each group (97%) underwent TAVI via the transfemoral approach, bicuspid patients were less likely to receive conscious sedation (57% vs 62%) and more likely to be treated with the largest 29-mm valve size (38% vs 30%; P < 0.0001 for both).
Rates of procedural complications, including conversion to open heart surgery, annulus rupture, cardiopulmonary bypass, aortic dissection, coronary obstruction, and the need for a second valve were low (0.5% or less) and did not differ between groups. These low rates were surprising, Makkar said.
All-cause mortality and stroke rates did not differ between bicuspid and tricuspid patients at any time point, although there was a numerically lower rate of mortality in the bicuspid group at 1 year.
Mortality and Stroke Rates
|
|
Bicuspid (n = 3,168) |
Tricuspid (n = 3,168) |
P Value |
|
All-Cause Mortality In-Hospital 30 Days 1 Year |
0.6% 0.9% 4.6% |
0.4% 0.8% 6.6% |
0.22 0.55 0.06 |
|
Stroke In-Hospital 30 Days 1 Year |
1.1% 1.4% 2.0% |
0.9% 1.2% 2.1% |
0.31 0.55 0.89 |
In terms of secondary endpoints, there were nonsignificantly higher rates of new pacemaker implantation in the bicuspid group at 30 days (7.9% vs 6.7%) and 1 year (8.9% vs 7.8%), as well as a greater need for aortic valve reintervention at 30 days (0.36% vs 0.13%; P = 0.07) and 1 year (1.16% vs 0.43%; P = 0.02), although rates were low overall.
“Despite the concerns for bad outcomes in patients with bicuspid aortic stenosis, at least in the analysis we did, these outcomes were very similar to what the published data are with surgical series, where the mortality is about 1% [at 30 days]. And these patients are much older, in fact, than some of the published data in surgical series,” Makkar said. He cautioned against reading too much into the lower mortality rate in bicuspid patients, but he said “it is very reassuring” and “gives me even more confidence in making a recommendation that in carefully selected patients with bicuspid [aortic stenosis], TAVR is a reasonable thing to do.”
Both the bicuspid and tricuspid groups had comparable increases in valve area and decreases in valve gradients. Moderate-or-severe paravalvular regurgitation tended to be higher in the bicuspid group at discharge (0.9% vs 0.3%; P = 0.0005), 30 days (1.8% vs 1.1%; P = 0.02), and 1 year (3.5% vs 2.1%; P = 0.36), something Abdel-Wahab said should be studied further in future prospective studies.
The overall score on the Kansas City Cardiomyopathy Questionnaire increased by almost 29 points in both groups by 30 days, with gains maintained through 1 year. NYHA class similarly reflected substantial improvements, with almost 95% of patients in class I or II by 30 days.
Where Are the Randomized Data?
Makkar said that in an ideal world a randomized trial would be conducted to prove the benefits of TAVI in patients with bicuspid disease, but he was skeptical about that actually happening.
Darren Mylotte, MD (Galway University Hospitals, Ireland), who was not involved in the study, agreed, telling TCTMD, however, that “the cat may already be out of the bag.” Medtronic’s Evolut platform already has CE Mark approval in Europe for use in patients with bicuspid disease who are at intermediate or worse risk of surgical mortality, he noted, and instructions for use of TAVI devices in the United States do not specifically state that bicuspid patients should not be treated, he pointed out.
“I can understand that there is some reluctance on the part of industry to perform these studies,” Mylotte said, noting that there is uncertainty about whether TAVI can match surgery in terms of 30-day rates of death and stroke. “But I think that it’s absolutely crucial to get them done,” Mylotte said.
Abdel-Wahab, too, sees a need for robust randomized data to guide decision-making around how to treat patients with bicuspid disease. Such a trial would have to be carefully designed to be fair to both TAVI and surgery based on what is currently known about the anatomical characteristics of bicuspid aortic stenosis, he stressed.
What to Watch Out for in Bicuspid Patients
While the field awaits robust randomized data, all three interventional cardiologists interviewed by TCTMD underscored the importance of careful patient selection when performing TAVI in the setting of bicuspid aortic stenosis.
Abdel-Wahab said the bicuspid patients in this study were likely very carefully selected for TAVI on the basis of anatomic characteristics. “They are at low risk, and they could be offered surgery with a very good outcome, so if we offer them TAVR we also need to make sure that they can be safely and effectively treated.”
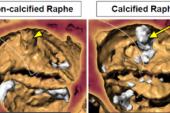
Anatomically, patients with bicuspid valves generally have more calcification and most, Mylotte said, have a raphe that is usually calcified or fibrotic. “That combination of calcium and raphe, especially if the raphe is elongated, can lead to more-difficult implantation and it can lead to malexpansion of the valve frame, be it with balloon-expandable or self-expanding devices,” he explained. “And both of those things can potentially make this a more-difficult procedure and with potentially a worse long-term outcome in terms of leaflet durability.” On top of that, these patients can have fragility in the aorta because of the nature of bicuspid disease, with about 40% ending up with dilated aortas.
“All in all, these patients can be more complex from a TAVI point of view. They require careful screening,” Mylotte said. “Valve selection and valve size selection is more challenging with bicuspid than tricuspid disease, and often the procedures themselves can be a bit more complicated in terms of predilatation, postdilatation, and so forth.”
It’s not surprising, then, that previous studies have shown that stroke has been more of an issue in bicuspid versus tricuspid disease, he said. “That wasn’t the case in this data set, which is great to see. Maybe we’re learning to do these procedures a little bit better. But when we know that surgery can perform very well in these patients, with death and stroke rates of 1% [at 30 days], that’s something that TAVI in bicuspid hasn’t been able to do thus far. . . . With TAVI we would have to prove that we can get to that bar, and maybe this is the first data set that suggests that with bicuspid we can.”
Much Longer Follow-up Needed
Without knowing about the anatomy of the bicuspid patients in this study, however, it is likely that the cohort represents procedures on the simpler end of the spectrum, Mylotte cautioned, noting that there could be unmeasured confounding at play, too.
“Therefore, I think the caveat is that while this is encouraging data, we need to evaluate on a case-by-case basis, and certainly we don’t know enough about the more-challenging anatomies to be recommending TAVI in all lower-risk patients with bicuspid aortic valve,” he advised. “We’re not there yet.”
Moreover, the field still lacks long-term data on the outcomes of TAVI in bicuspid patients, a crucial gap in knowledge, Mylotte said: “Of course in those younger patients, we need 10-year follow-up before we can decide whether or not it’s appropriate to treat these patients with TAVI versus surgery.”
For bicuspid disease, “where nonexpansion of the transcatheter heart valve, or indeed the fragility that’s associated with the aortic wall in some of these patients, can lead to longer-term issues, it’s really the longer term that we’re most interested in to see that these patients do as well with bicuspid morphology as tricuspid,” Mylotte said.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Makkar R. Outcomes of transcatheter aortic valve replacement for bicuspid aortic valve stenosis in the low-surgical risk population. Presented at: EuroPCR 2021. May 19, 2021.
Disclosures
- Statistical analyses were performed by Edwards Lifesciences.
- Makkar reports receiving grant/research support and consulting fees/honoraria from Abbott, Boston Scientific, Edwards Lifesciences, and Medtronic; and being a major stock shareholder or having equity in Entourage Medical.
- Mylotte reports consulting for Boston Scientific, Medtronic, and Microport.
- Abdel-Wahab reports no relevant conflicts of interest.


Comments