Half of TAVR Patients Develop Potentially Dangerous Conduction Abnormalities
New-onset BBB and a need for PPM should be considered serious adverse events, but not on the same scale as death or stroke, one expert said.
New-onset conduction abnormalities after TAVR are associated with increased risks of all-cause mortality and hospitalization for heart failure, according to a new study.
Plenty of research has been done looking at either bundle branch block (BBB) or permanent pacing after TAVR, but no consensus exists regarding the clinical consequences of these complications. Moreover, prior studies have primarily lumped patients with new-onset BBB and need for permanent pacemaker (PPM) together.
The most important aspect of the new study, lead author Troels H. Jørgensen, MD (Rigshospitalet, Copenhagen University Hospital, Denmark), told TCTMD, is that it divides up patients with left BBB, PPM, and those without any conduction abnormalities so that there is no overlap. “After separating those with new-onset left bundle branch block, I was surprised that there was such a huge impact on the late-term outcomes of having a permanent pacemaker as we saw in our study,” he said.
The paper, published in the January 14, 2019, issue of JACC: Cardiovascular Interventions, included 816 consecutive patients without pre-existing conduction abnormalities who underwent TAVR at a single Danish center between 2007 and 2017. At 30 days, 30.3% of patients were diagnosed with a new BBB without PPM and 16.2% had a new PPM.
After a median follow-up of 2.5 years, the risk of early all-cause mortality (< 1 year post-TAVR) was higher for the new BBB cohort but not the new PPM group compared with those with no conduction abnormalities. However, late all-cause mortality (≥ 1 year post-TAVR) was higher for patients with both new BBB and PPM compared with controls. Additionally, patients with new BBB and PPM reported a higher risk of hospitalization for heart failure over the study period.
Outcomes Compared With Patients with No Conduction Abnormalities
|
|
New BBB |
New PPM |
||
|
HR |
95% CI |
HR |
95% CI |
|
|
Early All-Cause Mortality |
2.80 |
1.18-3.67 |
1.64 |
0.72-3.64 |
|
Late All-Cause Mortality |
1.79 |
1.24-2.59 |
1.58 |
1.01-2.46 |
|
Hospitalization for Heart Failure |
1.47 |
1.02-2.12 |
1.66 |
1.09-2.54 |
Median hospital length of stay was longer for patients in the BBB (4.5 days) and PPM (4.0 days) compared with controls (3.0 days; P = 0.037). Also, LVEF dropped significantly from discharge to follow-up among patients in both the BBB and PPM groups (P < 0.001 for both) but not among those with no conduction abnormalities.
Turning to Prevention
“These conduction abnormalities . . . are not benign in the long term. They have severe consequences,” Jørgensen said, noting that there are no current treatments for them. “It seems like prevention is the better treatment really in clinical practice. Of course, we all aim to reduce the rate of new-onset conduction abnormalities, but I think maybe this study could put more emphasis that this rate needs to be taken down.”
Commenting on the study for TCTMD, Josep Rodés-Cabau, MD (Quebec Heart and Lung Institute, Canada), agreed that prevention will be key, especially as TAVR moves to lower-risk patients. While operators cannot change a patient’s age or anatomy, they can be more aware of patients who might be at greater risk for needing a PPM and then select patients and transcatheter valves accordingly, he suggested. Using ECG monitoring for a period of time might also be helpful in some patients.
“It's such a complex issue that is not easy, but this study overall points out that this problem is not solved and that we have to continue to try to improve all these issues,” Rodés-Cabau said.
In an accompanying editorial, Peter P.T. de Jaegere, MD, PhD (Erasmus University, Rotterdam, the Netherlands), Patrick Houthuizen, MD, PhD (Catharina Hospital, Eindhoven, the Netherlands), and Frits W. Prinzen, PhD (Maastricht University, the Netherlands), pose the question of whether new-onset conduction abnormalities after TAVR are either “innocent bystanders” or serious adverse events.
“There is currently debate and controversy as to whether TAVR-induced new conduction abnormalities, including new PPM, are associated with a dismal prognosis and whether they should be considered a serious adverse event or a complication,” they write. “This conflict is most likely due to the profound differences in the methods and definitions among studies, precluding a sound meta-analysis despite statistical methods to cope with heterogeneity.”
Because of this, “it may help to consider pathophysiologic observations. LBBB induces interventricular dyssynchrony, which in turn affects ventricular systolic and diastolic performance and may lead to increased end-systolic volumes, abnormal septal perfusion, and hypertrophy. Also, LBBB may progress to atrioventricular block and, therefore, sudden death,” the editorialists explain.
Ultimately, the findings underscore the question: “How much evidence do we still need before considering new LBBB and/or new PPM as an event that affects prognosis and quality of life and thus worthy to be considered a serious adverse event post-TAVR?” they conclude.
“I would most definitely think that [a new conduction abnormality] is an adverse event and it's not just an innocent bystander,” Jørgensen responded. “Of course, the results need to be confirmed in future studies with the same design, but there's a lot of other literature that would point in the same direction—that having these conduction abnormalities, either left bundle branch block or being paced in the right ventricle [leads] to complications.”
Rodés-Cabau agreed that there is “no doubt” that a new BBB or PPM after TAVR is a serious adverse event. “The problem is that, for example, some of these left bundle branch blocks will tend to disappear over time—not the majority, but some of them—and there are other studies . . . where the data is less strong in terms of association with poorer outcomes,” he said. “I think that there is a marker of risk, there's no doubt about that, but I don't think that we can put this at the same level of let's say dying or having a disabling stroke.”
Future research should focus on “really trying to make some modifications in the valve design [and] to maybe reduce this mechanical injury that is generated by the transcatheter valve,” Rodés-Cabau suggested. Also, “future studies should look at the specific strategies of treatment. It has to be more stratified, more predefined than it has been in the past in terms of what to do with the patients.”
Jørgensen said he would like to see “more long-term follow-up” to confirm these study findings, as well as prevention studies “perhaps potentially with cardiac resynchronization therapy in patients where conduction abnormalities do develop.”
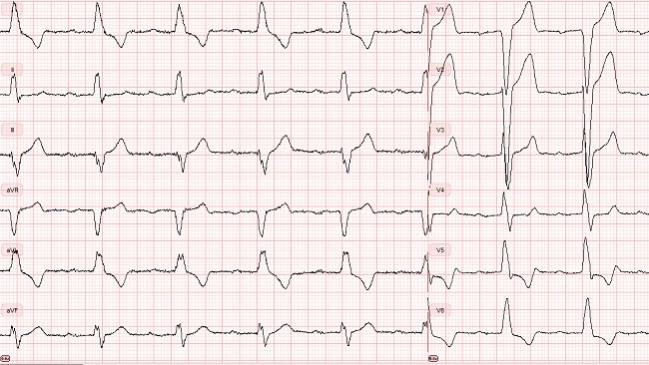
Photo Credit: Troels H. Jørgensen
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Jørgensen TH, De Backer O, Gerds TA, et al. Mortality and heart failure hospitalization in patients with conduction abnormalities after transcatheter aortic valve replacement. J Am Coll Cardiol Intv. 2019;12:52-61.
de Jaegere PPT, Houthuizen P, Prinzen, FW. New conduction abnormalities after transcatheter aortic valve replacement: an innocent bystander or a serious adverse event indeed? J Am Coll Cardiol Intv. 2019;12:62-64.
Disclosures
- Jørgensen reports receiving a research grant from Edwards Lifesciences.
- Rodés-Cabau, de Jaegere, Houthuizen, and Prinzen report no relevant conflicts of interest.


Comments