Hemodynamic Deterioration Post-SAVR: Dysmetabolic Profile, Calcification Could Be Early Warning Signs
Leaflet calcification, insulin resistance, and other factors up the risk of deterioration, which in turn raises the odds of death or reintervention.
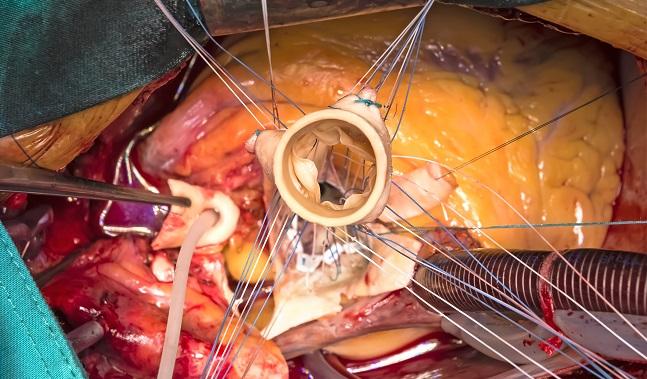
An observational study tracking patients for 10 years following surgical implantation of a bioprosthetic aortic valve prospectively shows that leaflet calcification and a dysmetabolic profile are associated with a higher risk of hemodynamic valve deterioration (HVD).
Calcification was also linked in the study to a 2.5-fold greater risk of death or reintervention during follow-up, whereas HVD quintupled the risk of these outcomes.
“We felt we should do a more [systematic] screening and analysis of the HVD based on Doppler echocardiography” in an unselected group of patients, senior author Philippe Pibarot, DVM, PhD (Laval University, Quebec City, Canada), told TCTMD. Importantly, he said, calcification was assessed using noncontrast CT, a simple imaging modality that can detect initial signs of mineralization without much radiation exposure.
Around 7 years after SAVR, approximately one-quarter of patients had leaflet calcification. “It’s already a sign that the valve is not normal,” Pibarot observed.
Michael Reardon, MD (Houston Methodist Hospital, TX), commenting on the study for TCTMD, said it’s an example of how the field is beginning to dig deeper into bioprosthetic valve failure. “This is great new information from [a research group] that has taught us so much about valve disease,” he said. “We’ve known for a long time that there’s an association between dyslipidemia and metabolic syndrome and progression of native valve and surgical valve [deterioration]. We’ve just never known if it’s causal.”
The mechanisms behind any causal relationships are likely to be complex, Reardon predicted. So far, there has been no evidence that treating these conditions with lipid-lowering drugs, for example, would prevent or slow valve changes. It may be that medications were started too late after SAVR, he suggested. “What we don’t know is if we started everybody on lipid-lowering drugs [whether] that would make a difference. There’s also more than one kind of valve used in [SAVR] and each kind of valve responds individually.”
Knowing more about early warning signs of deterioration will enable better patient management, Reardon and Pibarot agreed.
Clinical Consequences
Pibarot, with lead author Erwan Salaun, MD (Laval University and Aix-Marseille Université, Marseille, France), and colleagues, conducted a prospective longitudinal study tracking 137 patients who had undergone bioprosthetic valve surgery. Their results were published online July 9, 2018, ahead of print in the Journal of the American College of Cardiology.
At a median of 6.7 years after SAVR, patients were assessed with complete Doppler echocardiography to assess valve deterioration, multidetector CT to measure leaflet calcification, and a fasting blood sample to gauge their cardiometabolic risk. A median of 3 years later (nearly 10 years after SAVR), patients then underwent a second round of Doppler echo.
One-quarter of patients had leaflet calcification on the first round of imaging. Between that baseline imaging and follow-up echocardiography, 13.1% of patients developed HVD, defined as an annualized change in mean transprosthetic gradient ≥ 3 mm Hg/year and/or worsening or transprosthetic regurgitation by ≥ 1/3 class.
During clinical follow-up after the second imaging round, 38% of patients in the original cohort had experienced the primary composite endpoint of death from any cause or aortic reintervention (surgical replacement or transcatheter valve-in-valve). Leaflet calcification independently predicted the occurrence of a primary endpoint event (HR 2.58; 95% CI 1.35-4.82), as did HVD (HR 5.12; 95% CI 2.57-9.71).
Several factors predicted risk of HVD: leaflet calcification, insulin resistance (homeostatic model assessment [HOMA] index > 2.7), increased lipoprotein-associated phospholipase A2 (Lp-PLA2) activity (per 0.1 nmol/min/mL), and high PCSK9 level (≥ 305 ng/mL). These associations remained significant after adjustment for age, sex, and time since AVR.
Predictors of HVD: Univariate Analysis
|
|
OR |
95% CI |
|
Leaflet Calcification |
4.10 |
1.43-11.70 |
|
Insulin Resistance (HOMA > 2.7) |
3.30 |
1.19-9.23 |
|
Lp-PLA2 Activity (per 0.1 nmol/min/mL Increase) |
1.15 |
1.04-1.26 |
|
High PCSK9 Level (≥ 305 ng/mL) |
4.36 |
1.35-14.02 |
As to how these findings should impact care, Pibarot said that noncontrast CT should be considered as early as at 3 years and that any degree of calcification merits closer follow-up with Doppler echo as well as CT, which could then “be helpful to better determine the optimal timing to reintervene, potentially with a valve-in-valve.”
What to do with the biomarker findings is less clear, though evidence that a patient has diabetes or metabolic syndrome could inform risk stratification, Pibarot said. “We may be at the stage where we should consider doing some randomized clinical trials to test some pharmacotherapies,” such as PCSK9 inhibitors or strategies to improve insulin resistance, he suggested. Any intervention in these studies “should be done at day 1, after AVR, because the valve is still pristine. So it’s a good time to institute a pharmacotherapy and protect the valve.”
As pointed out in an editorial by George Thanassoulis, MD (McGill University Health Center, Montreal, Canada), biomarkers were measured in this study not before or immediately after surgery but at 5 to 9 years later, making it hard to tease out any potential cause-and-effect relationship with HVD. Study participants also weren’t recruited until years after their valve replacement, opening up the possibility of survivor bias.
Potential for Precision and Nuance
On the other hand, Thanassoulis writes, “a major strength of this study is the comprehensive analysis of several important risk factors including echocardiographic parameters, CT-based calcification, as well as metabolic biomarkers in all participants in an effort to determine the most relevant parameters that predict adverse valve outcomes post-AVR.” It provides a more complete picture, he says, than earlier studies that looked at many of these factors individually.
“As we enter the era of precision medicine, we will increasingly have the opportunity to use imaging, genomics, and blood-based biomarkers to clinically evaluate our patients with valvular heart disease,” Thanassoulis notes. “Such an approach, as demonstrated in the present study, could eventually identify the best candidates for bioprosthesis with the lowest risk for failure, and also point to therapeutic targets that modify key pathways in disease pathogenesis.”
Interest in valve deterioration has been growing with the advent of TAVR, Reardon and Pibarot observed to TCTMD.
“It has caused us to look at it in a more nuanced way,” said Reardon, a thoracic and cardiac surgeon. “Surgeons have always looked at valve failure as an ‘on/off’ proposition—we put a valve in you, and it was okay until it wasn’t. And when it wasn’t, we had to replace it. There wasn’t this nuanced ‘It’s starting to degenerate but still fine.’ Now that we have TAVR and valve-in-valve, we’re starting to look closer at how this progresses.”
Reardon suggested that further innovation may one day address deterioration, the Achilles’ heel of bioprosthetic valves. “If we had a biologic valve that lasted like mechanical valves and didn’t require coumadin, nobody would get a mechanical valve. People continue to work on [new ideas]. It may be how we treat the patient. It may be how we treat the valve. It may be different materials—we may eventually come up with an artificial material that has the pliability of a biologic material [but] doesn’t calcify, although that’s been kind of a lifelong dream.”
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Salaun E, Mahjoub H, Dahou A, et al. Hemodynamic deterioration of surgically implanted bioprosthetic aortic valves. J Am Coll Cardiol. 2018;72:241-251.
Thanassoulis G. Precision medicine for prosthetic valve deterioration: a glimpse into the future? J Am Coll Cardiol. 2018;72:252-254.
Disclosures
- Pibarot reports receiving research grants from Edwards Lifesciences and Medtronic for echocardiography core lab analyses in TAVR.
- Salaun reports no relevant conflicts of interest.
- Thanassoulis reports being a clinical research scholar funded by the Fonds de Recherche Sante-Quebec; participating in advisory boards for Ionis, Amgen, Sanofi, and Servier Canada; serving on speakers bureaus for Amgen, Sanofi, Servier, and Boehringer Ingelheim; and receiving research grants from Ionis, Servier Canada, the Canadian Institutes of Health Research, the Heart and Stroke Foundation of Canada, and the US National Institutes of Health.
- Reardon reports serving on an advisory board for Medtronic, as the national PI for the SURTAVI Low Risk and REPRISE III trials.


Comments