Hold the tPA? Study Probes Necessity of IV Thrombolysis Prior to Endovascular Therapy for Acute Stroke
The post hoc study should be interpreted cautiously, because it compares “apples and oranges,” one expert says.
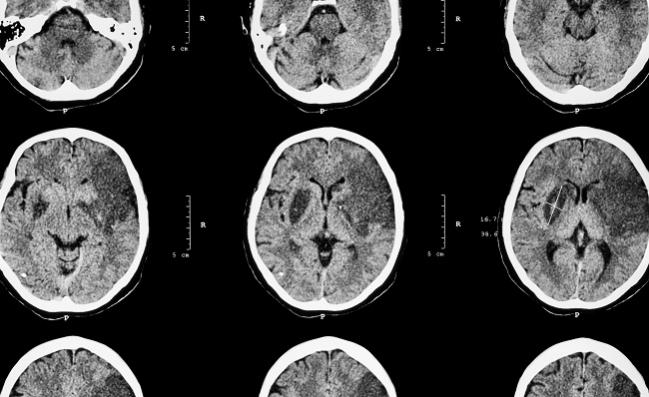
Standard practice dictates that all eligible patients receive IV thrombolysis before undergoing endovascular treatment of an acute ischemic stroke caused by a large vessel occlusion, but a new analysis of previously published data hints at the possibility of forgoing that initial step without harming outcomes.
Using pooled data from two randomized trials, researchers led by Jonathan Coutinho, MD (Amsterdam Medical Center, the Netherlands), found that none of the outcomes studied—including functional independence and mortality at 90 days—differed between patients who received IV thrombolysis before undergoing mechanical thrombectomy with a stent retriever and those who didn’t.
In the study, which was published online January 9, 2017, ahead of print in JAMA Neurology, “we don’t see an apparent benefit of IV tPA in those patients, but we should now move towards a proper clinical trial designed to address that question,” senior author Vitor Pereira, MD (Toronto Western Hospital, Canada), told TCTMD. He pointed out that the advantage of administering IV thrombolysis is that patients are treated early in the event that thrombectomy is delayed. But on the flip side, he said, the treatment adds cost and bleeding risk.
Pereira said his team and a group in Europe are already laying the groundwork for a trial to definitively assess whether IV thrombolysis is necessary before the procedure.
Commenting on the study for TCTMD, Michael Hill, MD (University of Calgary, Canada), said such a trial would be welcomed: “This is a good question, and it should be studied.”
The current study, however, should be interpreted cautiously, because it is “comparing apples and oranges,” Hill said, noting that patients who are or who are not eligible to receive thrombolysis are inherently different groups.
The stroke community is interested in exploring whether thrombolysis is needed before thrombectomy much like researchers in the coronary space previously studied whether such treatment is necessary before primary PCI in patients with ACS. Those investigations showed that pre-PCI thrombolysis did not carry a large benefit, but “my own view is that probably we’re not going to end up there” with stroke, Hill said, citing dissimilarities in the disease processes of stroke and ACS.
There is also emerging evidence, he said, that use of IV thrombolysis before endovascular treatment may help reduce the procedural complication of new distal infarcts. “People have perhaps a little bit of a romantic notion about thrombectomy, that it’s clean and it’s like taking a cork out of a wine bottle,” Hill explained. “But it’s kind of messy and the corks usually crumble, and we get fragments into the distal circulation.”
People have perhaps a little bit of a romantic notion about thrombectomy, that it’s clean and it’s like taking a cork out of a wine bottle. Michael Hill
Moreover, rates of complete reperfusion with thrombectomy are still under 80%, on average, which is not good enough to do away with IV thrombolytics, Hill argued. “If you could tell me that my interventional team could get the artery open 95% or 99% of the time, then I would have a lot less concern about withholding a therapy,” he said. But if the procedure is not effective in one out of every five patients, he added, “that’s a problem.”
Open Question
Several trials published in the past few years have established mechanical thrombectomy, primarily with newer-generation stent retrievers, as an effective treatment for patients with acute ischemic stroke caused by a large vessel occlusion in the anterior circulation. The vast majority of patients in those trials, however, received IV thrombolysis before the procedure, which has become established as standard practice. What benefit, if any, the approach adds to thrombectomy alone has not been directly studied in a randomized trial.
To take a preliminary look at the issue, Coutinho, Pereira, and colleagues pooled patient-level data from the SWIFT and STAR studies, both of which evaluated use of the Solitaire FR stent retriever (Medtronic Neurovascular). In both trials, IV thrombolysis was to be used in all patients who could receive it within 4.5 hours of the onset of stroke symptoms and did not have contraindications. Of the 291 patients included in the current analysis, 55% received IV thrombolysis.
Patients who received medical treatment before the procedure had a lower median ASPECTS score at baseline and were less likely to have diabetes and cardioembolic stroke attributable to A-fib.
There were no differences, however, in various procedural, clinical, and safety outcomes, including time from symptom onset to groin puncture, number of passes with the stent retriever, rate of successful reperfusion, emboli to new territory, functional independence or mortality at 90 days, and symptomatic or other types of intracranial hemorrhage. A difference in the unadjusted rate of vasospasm favoring thrombectomy alone became nonsignificant after multivariate adjustment.
The authors note that subgroup analyses of some of the recent trials, as well as a meta-analysis, did not indicate that the effect of thrombectomy differs based on the use of IV thrombolysis before the procedure.
In an accompanying editorial, Gursant Atwal, MD, and Adnan Siddiqui, MD, PhD (University at Buffalo, NY), agree with Hill and the study authors that the impact of thrombolysis should ideally be investigated in a randomized trial.
Nevertheless, they say, “the current study provides the largest independent core laboratory with a clinical endpoint committee- or a data and safety monitoring board-adjudicated prospective, multicenter dataset that highlights the question and provides critical data that can be used to design a definitive randomized clinical trial.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Coutinho JM, Liebeskind DS, Slater L-A, et al. Combined intravenous thrombolysis and thrombectomy vs thrombectomy alone for acute ischemic stroke: a pooled analysis of the SWIFT and STAR studies. JAMA Neurol. 2017;Epub ahead of print.
Atwal GS, Siddiqui AH. Mechanical thrombectomy for acute ischemic stroke: are we done? JAMA Neurol. 2017;Epub ahead of print.
Disclosures
- The study was sponsored by Covidien Neurovascular.
- Coutinho and Atwal report no relevant conflicts of interest.
- Hill reports serving as the principal investigator of the ESCAPE trial and receiving funding from Medtronic, Alberta Innovates, the Canadian Institutes of Health Research, and the Heart & Stroke Foundation of Canada.
- Siddiqui reports having financial interests in Buffalo Technology Partners, Cardinal, International Medical Distribution Partners, Medina Medical Systems, Neurotechnology Investors, StimSox, and Valor Medical; serving as a consultant to Amnis Therapeutics, Cerebrotech Medical Systems, CereVasc, Codman, Corindus, Covidien (acquired by Medtronic), GuidePoint Global Consulting, Lazarus (acquired by Medtronic), Medina Medical (acquired by Medtronic), Medtronic, MicroVention, Neuravi, Penumbra, Pulsar Vascular, Rapid Medical, Rebound Medical, Reverse Medical (acquired by Medtronic), Silk Road Medical, Stryker, The Stroke Project, Three Rivers Medical, and WL Gore & Associates; being a principal investigator or serving on the national steering committee for multiple related studies and trials; and being a member of the board of the Intersocietal Accreditation Committee.


Comments