Hybrid Approach to Reshaping Left Ventricle Offers Hope for HF Patients
Improvements in LV volume, QoL, and walking distance are seen with the nonsurgical therapy to reduce myocardial scarring.
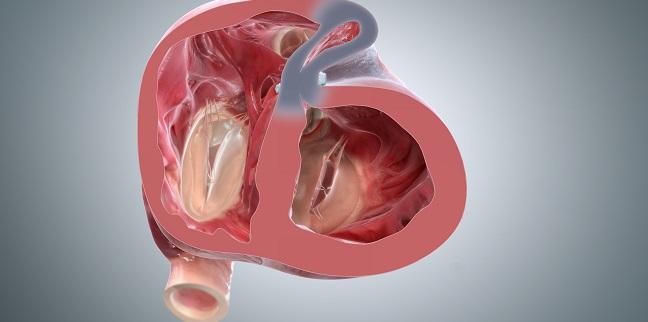
A less invasive alternative to surgical reconstruction improves symptoms and reduces left ventricular volume in patients with heart failure (HF) caused by MI, new data suggest. The procedure excludes myocardial scarring through a hybrid transcatheter and mini-thoracotomy technique.
“This could be an additional personalized therapy for a specific type of patient with HF after MI with scar tissue in the anteroseptal or apical wall of the left ventricle,” write Patrick Klein, MD (St. Antonius Hospital, Nieuwegein, the Netherlands), and colleagues.
Unlike surgical methods to reshape the damaged ventricle, this less-invasive approach does not require cardiopulmonary bypass, cardioplegic arrest, or ventriculotomy. Klein and colleagues initially employed a median sternotomy approach with the first-generation of the Revivent TC system (BioVentrix, San Ramon, CA) and then switched over to the hybrid technique with the second generation of the device.
Reporting 12-month results on 86 patients in the European Journal of Heart Failure, they observe that in addition to LV ejection fraction improvements, patients also had better quality of life (QoL) and improved walking distance.
Commenting on the study for TCTMD, Hemal Gada, MD (UPMC Pinnacle, Harrisburg, PA), said while more work needs to be done to establish reproducibility of the results and demonstrate a short and acceptable learning curve for the rather complicated technique, there is a need for this type of procedure.
“A lot of these patients get considered for LVAD therapy and heart transplantation, and then they either remain on lists for the rest of their lives where they're not treated or they are excluded for various different reasons, including age and operability,” he noted. “Making it a little bit more packageable in a tool kit, and having it rolled out in a standard way across multiple centers, showing procedural efficiency and safety, as well as good clinical outcomes, would be the next step.”
Significant Clinical, Functional Improvement
The study, which was conducted at 22 medical centers in 12 European countries enrolled patients with NYHA class II or III symptoms, LV dilatation and dysfunction from MI, and akinetic and/or dyskinetic transmural scarred myocardium.
The technique requires a series of steps, with an interventional cardiologist and a cardiac surgeon working together to first insert an introducer sheath into the right jugular vein. A snare is deployed into the right ventricular outflow tract to capture a wire introduced through the anterior wall of the left ventricle and septum. The snared wire is withdrawn from the jugular vein, and the Revivent TC’s internal hinged anchor is placed over the wire and advanced to the right side of the interventricular septum. Another anchor is attached from the epicardial surface. The scarred myocardium is then excluded by drawing the anchors together.
The study authors note that one important element of technique is that “the anchor pairs are set to a configuration parallel to the long axis of the heart. Each tether and the excluded portion of the scar are taken from the short axis of the heart. With this configuration, virtually all volume reduction decreases the radius of the left ventricle and is not just the result of amputation of an apical aneurysm.” They add that this method results in reduction in wall tension, reorientation of myofibers, and improvement in torsional dynamics, all of which likely contribute to functional improvement.
The first 51 patients enrolled were treated with the first-generation sternotomy approach, while the other 35 received the hybrid approach. Hybrid patients had shorter hospital stays, but there were no differences between the group in terms of major and minor adverse events. Ventricular arrhythmia (14%) and bleeding (8.1%) were the most frequent adverse events.
A lot of these patients get considered for LVAD therapy and heart transplantation, and then they either remain on lists for the rest of their lives [or] are excluded for various different reasons, including age and operability. Hemal Gada
Compared with baseline values, 12-month mean LV end-systolic volume index decreased by 27% (P < 0.001), mean LV end-diastolic volume index decreased by 24% (P < 0.0001), and mean LV ejection fraction increased by 16% (P < 0.005). Additionally, all patients had significant and sustained reductions in LV volume at 12 months.
NYHA class improved from 2.6 ± 0.5 at baseline to 1.9 ± 0.8 by 12 months (P < 0.001). The percentage of patients in NYHA class III declined from 59% at baseline to 22%. Mean 6-minute walk test distance improved by 21%, from an average of 363 m to 416 m (P < 0.001). QoL, as measured by the Minnesota Living with Heart Failure questionnaire, improved 34% from baseline (P < 0.001).
The researchers say their data also suggest that the procedure may have a positive effect in patients with functional mitral regurgitation (MR). Of 68 patients with measurable functional MR, average MR grade was reduced from a mean of 1.12 at baseline to 0.86 at 12 months. Due to these findings, Klein and colleagues suggest that this “should be considered as an additional potential benefit in patients who have MR but are not yet in need for mitral valve repair or replacement, or patients who have residual functional MR from previous repair of the mitral valve with ongoing progression of their HF symptoms.”
Taking Lessons From COAPT
In the past, the impact of left ventricular reconstruction has been mixed. In the STICH trial, for example, surgical ventricular reconstruction on top of CABG did not reduce mortality or HF hospitalization compared with CABG alone in patients with ischemic HF. But two STICH subanalyses, have shown a survival benefit in patients achieving a > 30% reduction in LV end-systolic volume index and/or postoperative LV end-systolic volume index < 60 mL/m2, and in those with smaller ventricles and ejection fraction ≥ 33%, Klein and colleagues say.
To TCTMD, Gada said the future of the therapy will come down to further refining the population most likely to benefit. Noting that procedure times can be up to 3 hours, he said identifying suitable anatomy that is not yet “too far gone” will require careful consideration.
“The way I would look at it is, take lessons from what COAPT showed us and look to what the TMVR trials are doing right now. Their inclusion criteria have changed,” he said. “So, instead of offering these types of therapies to EFs of 20%, bump your cutoff up to 30%. If you're talking about end-diastolic diameters, we know that patients who have a [LV end-diastolic diameter] of 8 centimeters tend to do worse with these types of therapies, so bring that cutoff down to 7 centimeters. I think we should probably also be more appreciative of hemodynamic factors as we look at randomized trials for this.”
Klein and colleagues say they have begun enrolling patients in a randomized trial that will compare the procedure to guideline-directed medical treatment.
Photo Credit: BioVentrix
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Klein P, Anker SD, Wechsler A, et al. Less invasive ventricular reconstruction for ischaemic heart failure. Eur J Heart Fail. 2019;Epub ahead of print.
Disclosures
- The study was sponsored by BioVentrix.
- Klein reports consultancy, proctoring and speaker agreements with BioVentrix and Edwards Lifesciences; and speaking fees from LivaNova.
- Gada reports no relevant conflicts of interest.


Comments