INTERACT4: Impact of Prehospital BP-Lowering May Depend on Acute Stroke Type
A neutral overall trial result seems to be due to harms in patients with cerebral ischemia and benefits in those with hemorrhages.
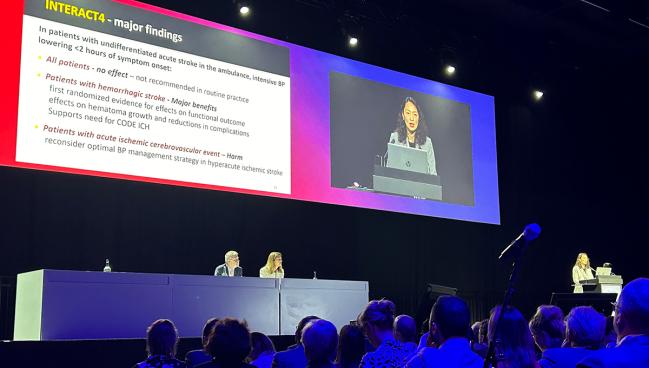
BASEL, Switzerland—Reducing blood pressure in patients with a suspected acute stroke in the ambulance before determining the specific stroke type does not provide a significant overall benefit, according to the results of INTERACT4 trial.
Functional outcomes at 90 days were no different between those who received immediate BP-lowering treatment and those who received usual care (common OR 1.00; 95% CI 0.87-1.15). However, the study cohort included a mix of hemorrhagic stroke and cerebral ischemia, with the intervention appearing to provide a clinical benefit in the former group and harm in the latter.
The findings were presented by Gang Li, MD, PhD (Shanghai East Hospital, Tongji University, China), and Lili Song, MD, PhD (The George Institute for Global Health China, Beijing, and University of New South Wales, Sydney, Australia), last week at the European Stroke Organisation Conference (ESOC) 2024. They were published simultaneously online in the New England Journal of Medicine.
Based on the overall result, lowering BP in the ambulance among patients with undifferentiated acute stroke “cannot be recommended in routine practice,” Song said.
The trial, however, provides the first randomized evidence suggesting that intensive BP-lowering can lessen bleeding in the brain and improve outcomes among patients with hemorrhagic stroke, which “provides strong justification” for pursuing the aims of Code ICH, she added. That initiative aims to improve the care of patients with intracerebral hemorrhage (ICH) using strategies similar to those that have been deployed in the treatment of acute ischemic stroke.
On the other hand, the findings also indicate that “we need to reconsider the optimal blood pressure management strategy in a hyperacute ischemic stroke,” Song said.
What makes this study unique from others by this research group, according to Jonathan Edlow, MD (Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, MA), who wrote an editorial accompanying the NEJM paper, is that the intervention was delivered before a CT scan could determine the type of stroke. That distinction is important in acute stroke because IV thrombolysis, for instance, shouldn’t be given to patients with hemorrhages.
The timing of BP-lowering in this trial—before the CT scan—needs to be considered when interpreting the results, he indicated. “To measure the effect of treatment on a disease, you have to make sure you have patients with that disease, and hemorrhagic stroke and ischemic stroke are two very different diseases,” Edlow told TCTMD.
Although in the US, Europe, and many parts of the world, hemorrhages usually make up about 20% of acute strokes, the proportion was closer to 50% in this trial. That, and the opposing effects of the intervention based on stroke type, explain the neutral result, he indicated.
Nonetheless, the results suggest that if a stroke can be definitively defined as hemorrhagic in the ambulance, the strategy explored here may be beneficial, Edlow said. “I think the preponderance of evidence is that it does help, and if we had a magic wand where we could tell this is a hemorrhage, I think that many doctors—if not most—would argue that lowering the blood pressure likely helps the patient.”
The INTERACT4 Trial
Earlier reperfusion treatment of acute ischemic stroke has been shown to improve outcomes over delayed treatment, Li said. He added that the impact of BP-lowering in patients with hemorrhagic stroke also is likely to be time-dependent, with most hematoma growth occurring in the first few hours.
Two prior trials testing the impact of prehospital transdermal glyceryl trinitrate to lower BP in patients presumed to have an acute stroke, RIGHT-2 and MR ASAP, failed to demonstrate benefits, with MR ASAP indicating the practice was harmful in the subset of patients with ICH. However, Li said, questions remain about whether different types of antihypertensive agents would influence the results and whether there are differential effects based on stroke type.
That led to the initiation of the INTERACT4 trial, which was conducted at 55 hospitals in two regions of China. Investigators randomized 2,404 patients (mean age 70 years; 38% women) who had a suspected acute stroke with an accompanying motor deficit (FAST score ≥ 2). All were assessed in the ambulance within 2 hours of symptom onset and had a systolic BP ≥ 150 mm Hg. They were randomized to immediate BP-lowering treatment (n = 1,205) or usual care (n = 1,199). Immediate treatment entailed up to two 25-mg IV boluses of urapidil to achieve a systolic BP of 130 to 140 mm Hg within 30 minutes, and usual care involved no antihypertensive therapy unless systolic BP exceeded 220 mm Hg. In-hospital BP management followed local guidelines in both groups.
The median time between symptom onset and randomization was 61 minutes, with a mean BP at randomization of 178/98 in both groups. Most patients underwent subsequent imaging to confirm stroke type, with 53.5% having cerebral ischemia and 46.5% having a hemorrhagic stroke.
The primary efficacy outcome was the distribution of modified Rankin Scale (mRS) scores at 90 days, with no overall difference between trial arms in terms of functional outcomes. That differed by stroke type, however.
Among patients with cerebral ischemia, functional outcomes were worse among those who received immediate BP-lowering treatment (common OR 1.30; 95% CI 1.06-1.60). The mortality rate was higher as well (23% vs 17%).
Opposite results were seen in patients with hemorrhagic strokes, with significantly better functional outcomes among those whose BP was lowered in the ambulance (common OR 0.75; 95% CI 0.60-0.92). Moreover, BP-lowering was associated with improved quality of life and a lower risk of death (24% vs 31%), fewer serious adverse events (27% vs 34%), and reduced relative hematoma growth at 24 hours (15% vs 21%). “So there was a biological mechanism of clinical effect,” Song said.
Move Faster for ICH
Craig Anderson, MD, PhD (The George Institute for Global Health, University of New South Wales), chair of the trial’s steering committee, discussed the implications of the INTERACT4 findings following the ESOC presentation. “As mentioned, this . . . for the first time provides us with that direct evidence that we’ve got to act quicker in intracerebral hemorrhage,” he said, noting that imaging in acute stroke has been focused on excluding hemorrhages so thrombolysis can be administered for cerebral ischemia. “We should be aiming to also identify intracerebral hemorrhage as quick as possible, because we have . . . a remarkable treatment effect here realized within a 20-minute transport time from the site to hospital.”
Meeting attendees who came to the microphone after the presentation alluded to the potential for mobile stroke units equipped with CT scanners and perhaps other tools yet to be developed that would enable clinicians to differentiate between hemorrhagic and ischemic strokes in the ambulance and facilitate BP-lowering in those with ICH.
“I think we’ve identified what the role should be in terms of blood pressure for ICH, and if we could find a way to do that, that would really change practice across the world,” Joseph Broderick, MD (UC Gardner Neuroscience Institute, Cincinnati, OH), said.
Edlow said that aside from CT scanners in ambulances—a capability available in only a few parts of the world—there are currently no other proven ways to identify stroke type in the prehospital setting.
“Given the current technology and practice in almost every place in the world, the prehospital phase of care is just too soon to know the information that one needs to rationally make a decision about aggressive blood-pressure control,” he said.
He predicted, however, that “there’ll be improvements probably in technology and imaging in order to make that hemorrhage-ischemia distinction earlier and earlier. And that helps because then you have a more clear diagnosis, you know whether the patient is eligible for one of the clot-busting thrombolytic drugs, you know how much you should reduce the blood pressure, and it gives you information about whether that ambulance should bring the patient to the local hospital or bypass the local hospital and go to a comprehensive stroke center.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Li G, Lin Y, Yang J, et al. Intensive ambulance-delivered blood-pressure reduction in hyperacute stroke. N Engl J Med. 2024;Epub ahead of print.
Edlow JA. Lowering blood pressure in stroke patients in the ambulance – a bridge too close? N Engl J Med. 2024;Epub ahead of print.
Disclosures
- INTERACT4 was supported by a grant from the National Health and Medical Research Council of Australia; a seed grant for research in underserved populations of low-middle-income countries from the George Institute for Global Health; grants from Shanghai East Hospital of Tongji University, including grants from the Shanghai Key Clinical Discipline, the Construction Project of Key Discipline Groups of Shanghai Pudong Health Bureau, the Clinical Plateau Discipline Construction Project of Shanghai Pudong New Area Health Committee, the Pilot Program of East Hospital Affiliated to Tongji University, the Shanghai East Hospital Clinical Research Special Project, and the Stroke and Dementia Special Fund of Shanghai Science and Technology Development Foundation; grants in Chengdu, including grants from the National Natural Science Foundation of China, the Sichuan Science and Technology Program, the Project of Neurology Key Discipline of Sichuan, the Chengdu Science and Technology Bureau, the talent fund of Sichuan Provincial People’s Hospital, and the talent fund of the First Affiliated Hospital of Chengdu Medical College; and Takeda Pharmaceuticals China.
- Anderson reports grants/contracts from the Medical Research Council, the Medical Research Foundation of the UK, the National Health and Medical Research Council, Penumbra, and Takeda California.
- Song reports grants/contracts from Takeda China and the George Institute for Global Health.
- Li reports no relevant conflicts of interest.
- Edlow reports being UpToDate’s section editor for neurological emergencies.





Comments