Left Bundle Branch Area Pacing May Lessen Arrhythmias in CRT Patients
Increased reverse remodeling compared with biventricular pacing may explain the finding, but randomized confirmation is needed.
PHILADELPHIA, PA—For patients treated with cardiac resynchronization therapy, use of left bundle branch area pacing (LBBAP) appears to lower arrhythmic risk compared with conventional biventricular pacing, an analysis of the observational International Collaborative LBBAP Study (I-CLAS) shows.
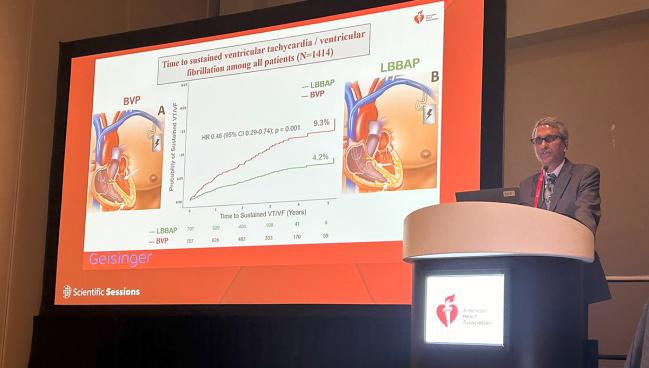
Those who underwent LBBAP had lower rates of sustained ventricular tachycardia and fibrillation (VT/VF) and new-onset atrial fibrillation (AF) during a mean follow-up of 32 months, Pugazhendhi Vijayaraman, MD (Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA), reported here recently at the American Heart Association 2023 Scientific Sessions.
The findings, published simultaneously online in Circulation, indicate that “physiologic resynchronization by left bundle branch area pacing, with greater reverse remodeling, may be associated with lower risk for arrhythmias compared with biventricular pacing,” Vijayaraman concluded.
He and his colleagues note, however, that this “needs to be confirmed in randomized clinical trials.”
Arrhythmias in I-CLAS
Conduction-system pacing—which includes LBBAP and His-bundle pacing—appears to be a safe and effective alternative to biventricular pacing in patients with CRT devices, although randomized data remain sparse. In particular, Vijayaraman said, there’s increasing evidence from large observational studies and small randomized trials that indicates LBBAP is an “excellent physiologic alternative” to biventricular pacing, providing a greater increase in LVEF and possibly a reduction in hard clinical outcomes like death or heart failure hospitalization, as seen in the main I-CLAS results published earlier this year.
The current analysis zeroes in on risks of various arrhythmias with the two types of pacing in I-CLAS, a nonrandomized, retrospective study conducted at 15 international centers. It included patients with an LVEF of 35% or less, NYHA class II-IV heart failure symptoms, and a class I or II indication for CRT (with successful device implantation).
In the overall cohort of 1,778 patients, those treated with LBBAP versus biventricular pacing were more likely to be female, had a higher rate of nonischemic cardiomyopathy, and were less likely to have left bundle branch block and to be treated with amiodarone. Investigators used propensity-score matching to even out those differences, resulting in 707 matched pairs of patients (mean age 69 years; 33% women).
One of the primary endpoints of the analysis was sustained VT or VF, with a lower rate seen in the LBBAP versus biventricular pacing group (4.2% vs 9.3%; HR 0.46; 95% CI 0.29-0.74). Results were similar in an analysis confined to patients with no prior history of either of those arrhythmias or of antiarrhythmic drug use.
The other primary endpoint was new-onset AF lasting more than 30 seconds, and this, too, was less frequent in the LBBAP group (2.8% vs 6.6%; HR 0.34; 95% CI 0.16-0.73).
Among secondary endpoints, LBBAP was associated with significantly lower rates of any ventricular arrhythmias, including both nonsustained and sustained VT/VF (7.8% vs 15.1%); implantable cardioverter-defibrillator shocks (3.3% vs 7.2%); VT storm (0.8% vs 2.5%); AF lasting more than 6 minutes (1.8% vs 5.1%); and AF lasting more than 24 hours (0.7% vs 2.9%).
The investigators also performed a responder analysis based on the proportion of patients who had at least a 5% improvement in LVEF. Among responders, LBBAP was associated with a significantly lower rate of sustained VT/VF compared with biventricular pacing (2.7% vs 7.3%; HR 0.33; 95% CI 0.15-0.74). There was a similar trend in nonresponders, although the difference didn’t reach statistical significance (7.2% vs 14.8%; HR 0.51; 95% CI 0.25-1.06).
Many Questions Remain
Discussing the results after Vijayaraman’s presentation, Jodie Hurwitz, MD (North Texas Heart Center, Dallas), president of the Heart Rhythm Society, called the lower rates of VT/VF and new-onset AF in patients treated with LBBAP “impressive.”
As for why arrhythmia risk would be reduced with LBBAP, she proposed several possibilities:
- It may deliver more-physiologic activation of the ventricles
- Epicardial coronary venous pacing with biventricular pacing could be proarrhythmic
- LBBAP may be better than biventricular pacing for patients with right bundle branch block or intraventricular conduction delay
- There were more nonresponders in the biventricular group
- Biventricular pacing can be associated with a higher incidence of VT/VF storm after implant
- Increased reverse remodeling with LBBAP could reduce rates of AF
Additional questions that need to be answered in future studies, she said, include whether women do better than men with LBBAP, which has been seen with biventricular pacing; whether differences in arrhythmia risk between the two pacing modalities has to do with differences in the types of cardiomyopathy and conduction disturbances affecting the treated patients; and whether the results of the current analysis would apply to a broader population of electrophysiologists.
“I actually have to impress upon everybody that this group of people are really, really good at placing these left bundle area pacing leads, and will this really translate to all of us everywhere?” Hurwitz said.
Vijayaraman acknowledged the limitations of the study and specified that its findings were hypothesis-generating. He said the Left vs Left trial, a randomized comparison of conduction-system pacing and biventricular pacing, will hopefully be able to provide answers to a lot of the remaining questions.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Herweg B, Sharma PS, Cano O, et al. Arrhythmic risk in biventricular pacing compared with left bundle branch area pacing: results from the International Collaborative LBBAP Study (I-CLAS). Circulation. 2023;Epub ahead of print.
Disclosures
- Vijayaraman reports honoraria, consulting fees, and research/fellowship support from Medtronic; consulting fees from Abbott and Eaglepoint LLC; honoraria from Boston Scientific; and a patent for a His-bundle pacing tool.
- Hurwitz reports no relevant conflicts of interest.




Comments