Lipid-Rich Plaque in Nonculprit Regions of the Target Vessel Predicts Future MACE Risk
The findings argue for secondary prevention to treat the overall patient rather than make the case for intervening on nonculprit plaques.
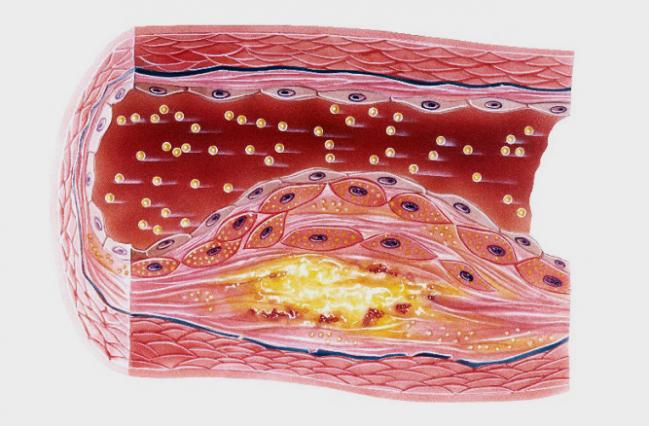
For patients undergoing PCI, the presence of lipid-rich plaque in nonculprit regions of the target vessel on optical coherence tomography (OCT) foretells a doubling in the risk of nonculprit MACE in subsequent years, according to a new study. However, most of those events are revascularization for recurrent ischemia, and experts cautioned to TCTMD that the results should not inspire operators to seek out and treat these plaques.
“I am against the local approach,” stressed Ik-Kyung Jang, MD, PhD (Massachusetts General Hospital, Boston, MA), senior author of the paper published online today in the Journal of the American College of Cardiology. “[Finding] lipid-rich plaque does not indicate that that [particular plaque] has to be treated, he said. “It is just a marker signifying that this patient is at high risk and therefore we have to focus on more aggressive secondary prevention, such as cholesterol-lowering therapy,” as well as on close follow-up.
Similarly, Marc Dweck, MBBS, PhD (University of Edinburgh, Scotland), who was not involved in the study, told TCTMD that when interpreting these results, it’s better to think at the patient level than at the lesion level.
The fact that the lipid-rich plaques were so common—witnessed in 33.6% of patients—yet events were so rare, he said, means that most did not cause clinical harm. “That really questions any sort of strategy that would look to stent individual lesions on the basis of their plaque characteristics,” Dweck commented.
Twice the Risk of MACE
Jang, along with lead author Lei Xing, MD, PhD (Second Affiliated Hospital of Harbin Medical University, Harbin, China), and others included 1,474 PCI patients treated at 20 sites in six countries as part of the Massachusetts General Hospital OCT Registry. Follow-up lasted as long as 4 years (median 2 years).
There were 74 instances of MACE, amounting to an overall rate of 7.1%; these included 66 ischemia-driven revascularizations, five cardiac deaths, and 21 acute MIs. Events stemming from the culprit lesion occurred at a rate of 2.6%, and nonculprit-lesion events occurred at a rate of 4.3%. By 48 months, the rate of nonculprit MACE was higher in the one-third of patients with lipid-rich plaque than in those who lacked it (7.2% vs 2.6%; P = 0.033).
Lipid-rich plaque in nonculprit regions was associated with double the risk of future MACE (RR 2.06; 95% CI 1.05-4.04). Other independent predictors of events during follow-up were ACS at index presentation (RR 2.54; 95% CI 1.25-5.17) and interruption of statin use ≥ 1 year (RR 4.52; 95% CI 1.92-10.61).
The lipid-rich plaques of patients who had nonculprit events tended to have longer lipid lengths, wider maximal lipid arcs, and smaller minimal lumen areas compared with those of patients who did not experience MACE.
Looking Toward the Future
In an editorial accompanying Xing et al’s paper, Gary S. Mintz, MD (Cardiovascular Research Foundation, New York, NY), observes that it’s still uncertain which form of imaging—OCT alone or with the addition of spectroscopy, IVUS, or near-infrared spectroscopy—is best at detecting and quantifying lipid.
Moreover, much like Jang and Dweck, he is circumspect about the clinical applications. The study’s low nonculprit event rate “raises the question of whether an invasive imaging strategy to detect and treat vulnerable plaques or vulnerable patients makes sense in the current era of modern stents and modern antiatherosclerotic therapies, especially because 20% of the patients in the nonculprit MACE group were not taking statins and interruption of statin use for longer than 1 year was an independent predictor of MACE,” Mintz writes.
“Conversely, absence of an OCT-detected [lipid-rich plaque] did not give the patient a clean bill of health during the follow-up period,” he points out.
For now, Jang said, OCT imaging of nonculprit regions is mainly a research tool, though it’s possible that in the future the approach could be used for risk stratification.
In the United States, intravascular imaging is used during roughly 15% of PCI cases, Jang reported, whereas he uses it 70% of the time. Other regions of the world employ some form of intravascular imaging to various degrees—in Japan, for example, its use reaches higher than 90%, Jang estimated. “I use OCT to optimize PCI, and rather than throw away this additional information [on nonculprit plaques] I tried to collect it and see how it [might inform] better patient care,” he added.
Dweck, while seeing a potential for risk stratification based on OCT, saw no immediate impact on practice. “Ultimately, what we need is big prospective studies to see if imaging these plaques adds anything on what we’re already doing in terms of assessing risk factor scores and [doing] imaging assessments of plaque burden that are simpler,” he advised.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Xing L, Higuma T, Wang Z, et al. Clinical significance of lipid-rich plaque detected by optical coherence tomography: a 4-year follow-up study. J Am Coll Cardiol. 2017;69:2502-2513.
Mintz GS. Predicting the vulnerable patient using intravascular imaging. J Am Coll Cardiol. 2017;69:2514-2516.
Disclosures
- Jang reports receiving grants and consulting fees from St. Jude Medical.
- Mintz reports receiving honoraria and grant or fellowship support from Boston Scientific, St. Jude Medical, Volcano, and ACIST Medical Systems.
- Xing and Dweck report no relevant conflicts of interest.


Comments