Low Bleeding Profile With Asundexian Seen in Pooled Analysis
Low bleeding liability with the XIa inhibitor may mean higher doses are possible, boosting efficacy, one investigator suggested.

Cumulative safety data from three trials testing the reversible direct factor XIa inhibitor asundexian in patients at risk for stroke or recurrent cardiovascular events suggest a better bleeding profile compared with apixaban (Eliquis; Bristol Myers Squibb) in a variety of patient types.
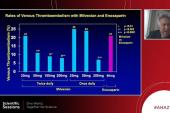
The three phase II trials—PACIFIC-AF, PACIFIC-AMI, and PACIFIC-STROKE—were not designed to evaluate efficacy for thromboembolic events or powered to detect differences in bleeding between asundexian doses or between asundexian and placebo. Pooling them in the meta-analysis showed that at both the 20-mg and 50-mg doses, asundexian was associated with consistently fewer types of all ISTH bleeding than apixaban 5 mg.
“The most important takeaways are that at the doses studied, the bleeding rates are very low and I think do suggest that the liability of the bleeding expectation is low,” the study’s senior author Marc P. Bonaca, MD, MPH (University of Colorado School of Medicine, Aurora), told TCTMD.
Even in patients on dual antiplatelet therapy (DAPT), the addition of asundexian produced little to no extra burden of bleeding, the analysis showed.
“We think that these data, although early days, are supportive of the safety of a factor XI-based approach,” Bonaca added.
However, as TCTMD reported in November 2023, the efficacy of asundexian in atrial fibrillation (AF) is in question given that the phase III OCEANIC-AF trial of asundexian versus apixaban was unexpectedly halted for lack of efficacy. The phase III OCEANIC-STROKE trial is continuing, but in patients who have already had a stroke or transient ischemic attack.
To TCTMD, Bonaca said the bleeding data may be an important part of this story since dose selection in the trials was based on modeling data.
“I think these [bleeding] data suggest that we could probably push to an even higher dose of asundexian,” he noted. “Given that you're not seeing bleeding at the doses studied, one question would be: could you then study a higher dose that might be more efficacious in the A-fib setting?”
Pooled Analysis Results
For the study, published recently in the Journal of the American College of Cardiology, researchers led by John W. Eikelboom, MBBS, MSc (Population Health Research Institute, Hamilton, Canada), sought to evaluate the effect of asundexian at three doses (10 mg once daily, 20 mg once daily, and 50 mg once daily) on bleeding at different severities and sites in the 4,164 patients pooled from the three studies. The mean age of AF patients (n = 755) was 73.7 years, with a slightly lower mean age of 67 years in those with prior MI or stroke (n = 3,409).
Of the more than 500 ISTH bleeding events that occurred, the most common were GI, respiratory, urogenital, and skin, with the most incidents reported in the first 30 days in those with AF and in the first 90 days in patients with recent MI and stroke history.
We think that these data, although early days, are supportive of the safety of a factor XI-based approach. Marc P. Bonaca
Compared with apixaban, the HR for all bleeding types for pooled asundexian doses was 0.40 (90% CI 0.25-0.65). Asundexian also was associated with numerically lower frequencies and incidence rates of the composite of ISTH major or clinically relevant nonmajor (CRNM) bleeding (HR 0.33; 90% CI 0.11-0.94), as well as minor bleeding (HR 0.46; 90% CI 0.27-0.77). There were no patients with ISTH major bleeding events.
At all doses studied, asundexian was associated with similar rates of major and all bleeding as placebo in patients with recent MI or stroke. The only exception was the 50-mg dose, which was associated with a higher rate of CRNM bleeding (HR 1.48; 90% CI: 1.02-2.16).
“Treatment effects appeared to be consistent irrespective of age, renal function, history of coronary artery disease, history of TIA or stroke, or history of bleeding except in the asundexian 10 mg versus placebo group, where bleeding appeared to be increased in patients with prior TIA or stroke but not in those who did not have prior TIA or stroke,” Eikelboom and colleagues write.
Small Molecule Inhibitors Act Differently
In an accompanying editorial, Felicita Andreotti, MD, PhD (Fondazione Policlinico Universitario A. Gemelli IRCCS , Rome, Italy), and colleagues note that the analysis also shows no significant association between asundexian exposure, measured as area under the curve (AUC), maximum or minimum plasma concentration, and major or CRNM bleeding.
“This rather surprising finding may reflect [factor XI] physiology, heterogeneity across studies (eg, for age, sex, bleeding history, asundexian dose, DAPT), and/or limited traumatic or surgical bleeding triggers,” they write. “Another possibility is that the three doses of asundexian are low on the dose-response curve, showing excellent safety but exposing to low efficacy because of underdosing.”
While Andreotti and colleagues admit that the discontinuation of OCEANIC-AF casts a shadow on the promise of asundexian in patients with AF, they suggest that future factor XIa inhibitor development “may include clinical challenges that have been neglected so far, in particular the prevention of thrombotic complications in patients with cardiac devices or prostheses.”
For Bonaca, the data so far on asundexian as well as the other factor XI inhibitors abelacimab and milvexian are pointing toward drug-specific mechanisms in this new world of small molecule agents.
“Just saying that one of these drugs works doesn’t [mean] you can extrapolate because each drug needs to do its dose finding and that is still ongoing,” he said. “Factor XI may be different than other agents in the coagulation cascade. Even with factor X, you have to [balance] benefit/risk because there is a bleeding liability. Factor XI is just fundamentally different, it appears. For asundexian, you can very much inhibit factor XI [but] something different is happening with the small molecule because we’re not seeing that bleeding liability.”
Bonaca added that the halting of OCEANIC-AF doesn’t necessarily mean the end of the efficacy question for asundexian, although even at higher doses it might not be the right agent for first-line therapy in patients with AF. But even if it isn’t, the low risk of bleeding may make it attractive to the many patients who otherwise refuse anticoagulation therapy.
“We know there are a lot of patients who won’t take [anticoagulants] because they worry about bleeding,” he said. “If you had a drug that was efficacious, maybe not as efficacious as apixaban, but didn't cause bleeding, and if you're unwilling to take any of the existing agents because of bleeding risk, it still might be better to be on that than nothing.”
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Eikelboom JW, Mundl H, Alexander JH, et al. Bleeding outcomes in patients treated with asundexian in phase II trials. J Am Coll Cardiol. 2024;83:669-678.
Andreotti F, Massetti M, Montalescot G. Thrombosis, bleeding, and the promise of factor XI(a) inhibition. J Am Coll Cardiol. 2024;83:679-681.
Disclosures
- Eikelboom reports honoraria, fees, or research grants from Anthos, Bayer, Boehringer Ingelheim, Bristol Myers Squibb, DSI, Idorsia, Janssen, Merck, Pfizer, and Servier.
- Bonaca reports modest stock holdings in Medtronic and Pfizer; and has received consulting fees from Audentes.
- Andreotti reports consulting/lecture fees from Amgen, AstraZeneca, Bayer, BMS/Pfizer, Daiichi Sankyo, and Servier.



Comments