Mortality Risk Varies Among Patients With Very High LDL Levels
In this high-risk group with LDL levels ≥ 190 mg/dL, researchers also spotted a concerning trend of declining statin use.
Not all patients with severe hypercholesterolemia are the same—that’s the message from a large analysis of a racially and ethnically diverse US population showing that some of these individuals are at a higher risk for all-cause mortality than others.
Males, older people, and those with various comorbidities, including hypertension, diabetes, and prior MI, for example, were all at a significantly elevated risk of mortality over longer-term follow-up, report investigators.
“Patients with LDL cholesterol greater than 190 [mg/dL], those with severe hypercholesterolemia, have traditionally been categorized as high risk without any need for further risk stratification,” senior investigator Leandro Slipczuk, MD, PhD (Montefiore Healthcare Network/Albert Einstein College of Medicine, Bronx, NY), told TCTMD. “We’re supposed to use a statin, which has proven benefit in these patients, with no further reclassification recommended, but there’s now multiple studies showing these patients have a heterogeneous risk for atherosclerotic cardiovascular disease [ASCVD].”
In this study, published online November 16, 2023, in Circulation, investigators observed some troubling trends, noting that statin use declined over the 10-year study period.
“The alarming thing here, in particular, is in primary prevention,” said Slipczuk. “I think these patients are undertreated, which we think might be because it’s not recognized that these patients are really at high risk.”
Statin Usage Too Low
In the present study, investigators wanted to assess the differential risks of ASCVD in a diverse population with severely elevated LDL cholesterol levels. They point out that different racial and ethnic groups have been historically underrepresented in previous studies.
The analysis included 18,740 patients (mean age 53.9 years; 38.1% female) enrolled in the Montefiore Health System between 2010 and 2020 who had at least a single LDL cholesterol measure of 190 mg/dL or greater. Of those included, 37% were non-Hispanic Black, 30% were Hispanic, 12% were non-Hispanic white, and 2% were non-Hispanic Asian.
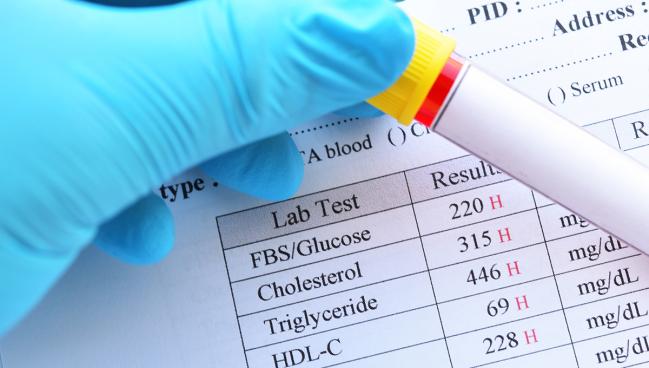
Nearly half of patients had hypertension (47%) while diabetes was present in one-third of patients (31%). Additionally, 20% had chronic kidney disease, 29% were smokers, and 11% had preexisting CAD. The mean baseline LDL and total cholesterol levels were 212 and 298 mg/dL, respectively. Three-quarters of patients were on statins, including 93.0% for secondary prevention. For those with preexisting CAD, 14.9% were prescribed ezetimibe and 4.7% were on a PCSK9 inhibitor.
At 9-year follow-up, all-cause mortality was 9.3%, 8.5%, 6.9%, and 6.1% in the non-Hispanic Black, white, Hispanic, and Asian patients, respectively. Higher LDL-cholesterol levels were associated with a higher risk of mortality, but a U-shaped curve was observed for HDL cholesterol, with the lowest mortality seen in those with levels between 45 and 80 mg/dL. A similar U-shaped curve was evident with body mass index (BMI), where mortality was higher for those with BMIs less than 27 and greater than 40 kg/m2.
In a multivariate analysis, there was no significant difference in the risk of death at 9 years in the non-Hispanic Black and Asian patients compared with non-Hispanic white patients, but Hispanic patients did have a lower risk (adjusted HR 0.73; 95% CI 0.55-0.96).
Overall, male sex (adjusted HR 1.31; 95% CI 1.09-1.58), older age (adjusted HR 1.19 per 5-year increase; 95% CI 1.15-1.23), and low BMI (adjusted HR 3.36; 95% CI 2.29-4.99) were associated with a significantly increased risk of death at 9 years. Additionally, the presence of hypertension, chronic kidney disease, diabetes, heart failure, and MI were each individually associated with a higher risk of death. The higher risk of mortality seen in those with a low BMI (< 20 kg/m2) is likely because being underweight is a marker for some other chronic illness, such as cancer or heart failure, said Slipczuk.
In an analysis stratifying patients with a possible, probable, and definite familial hypercholesterolemia (FH) diagnosis using the Dutch Lipid Clinical Network criteria, the mortality rate at 9 years for those with possible FH was 3.9%, whereas it was 21.9% and 38.7% for those with probable and definite FH, respectively.
“Once you have familial hypercholesterolemia, you are exposed to very high LDL-cholesterol levels from an earlier age,” said Slipczuk. “So, you’re at an even higher risk.”
Declining Statin Use
Finally, the group looked at changes in statin use over time. In the most recent time period (2019-2020), 56% of patients without preexisting disease were on statins compared with 85% for secondary prevention. However, there was a decline in statin use over time, particularly in primary prevention, which was down from a high of 80% in 2010-2012. Overall, 55.3% of patients had LDL levels of 130 mg/dL or greater and only 21% got below 100 mg/dL. Just 7% of patients had an LDL level less than 70 mg/dL.
“We know how to treat hypercholesterolemia,” said Slipczuk. “We have statins that have proven benefits, and we have multiple other medications that can help decrease LDL cholesterol, which we know is the biggest link to coronary and atherosclerotic cardiovascular disease. Yet we're still not doing a good job, and not just in this cohort, but we see that in multiple cohorts.”
Treatment inertia and difficulties accessing care are possibilities that might explain the statin treatment rates. At their center, multiple efforts are underway to address treatment gaps, including attempts to increase referrals to centers with specialty lipid clinics. The group has also started a bedside program for PCSK9 inhibitors for cardiac patients with LDL cholesterol levels exceeding US guideline targets in need of further lowering, he said.
In terms of clinical implications, Slipczuk said their new data should help physicians be more aggressive in targeting those patients with severe hypercholesterolemia and other risk factors, such as diabetes and hypertension. In a study published last year, the researchers previously showed that calcification—either in the coronary arteries or thoracic aorta—was also associated with a higher risk of mortality in patients with severe hypercholesterolemia.
“So, there’s different tools,” said Slipczuk, referring to myriad ways physicians can tease out the risk of patients with very high LDL cholesterol.
Earlier this month, researchers, including Slipczuk, published a study showing that more than one-quarter of patients with LDL cholesterol levels 190 mg/dL or greater were unaware of their high cholesterol and were untreated. The prevalence of severe hypercholesterolemia declined over a 20-year period in that study, although progress was quite slow.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Miles J, Scotti A, Castagna F, et al. Long-term mortality in patients with severe hypercholesterolemia phenotype from a racial and ethnically diverse US cohort. Circulation. 2023;Epub ahead of print.
Disclosures
- Slipczuk reports receiving consulting honoraria from Philips and Amgen; participating in an advisory board meeting from BMS; and receiving institutional grant support from Amgen and Philips. He was the site principal investigator for the Victorian-INITIATE trial.





Comments