New Antithrombotic Revacept Fails to Reduce Myocardial Injury in PCI
The novel, lesion-directed GPVI antagonist, however, was safe and will next be tested in a higher-risk cohort, investigators say.
A phase II trial of a novel, lesion-directed antithrombotic agent shows no effect on preventing myocardial injury in low-risk patients undergoing PCI, but the safety profile was good with few bleeding events. Trialists believe the disappointing results don’t rule out a role for the agent in higher-risk settings.
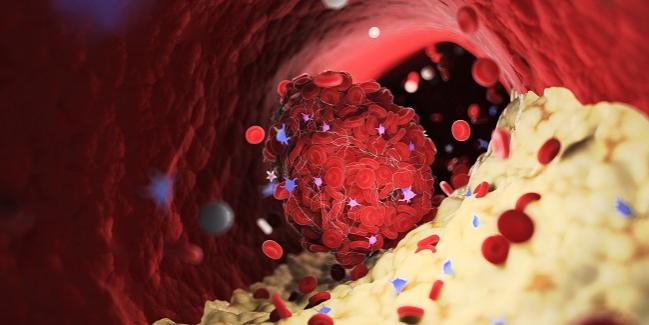
Revacept (advanceCOR), an intravenous, competitive antagonist to platelet glycoprotein VI (GPVI), efficiently binds to collagen and effectively mimics the GPVI pathway, blocking platelet aggregation. The appeal of the agent stems from prior studies suggesting that it would permit
fast and powerful platelet inhibition at the site of the atherosclerotic plaque injury, without increasing the risk of bleeding more systemically. Past research has shown limited success with a similar agent derived from snake venom.
“Collagen normally is covered by endothelial cells, but when you have plaque rupture in coronary arteries, for example, collagen becomes exposed and this is a major trigger of clot formation,” explained senior author Steffen Massberg, MD (Ludwig-Maximilian University of Munich, Germany). “Consequently, if you block bad binding of platelets to collagen you prevent clot formation.”
In contrast to something like the glycoprotein IIb/IIIa pathway, GPVI “appears to have a less-important role in the physiologic setting,” Massberg told TCTMD. “If you block GPVI, the effect on bleeding time is very moderate. It's not without an effect, but it's much less pronounced compared to the drugs that are used so far. And that is because GPVI appears to play a minor role in hemostasis.”
Safety Shown
For the ISAR-PLASTER study, published online March 31, 2021, in JAMA Cardiology, Massberg, along with lead author Katharina Mayer, MD (Deutsches Herzzentrum München, Munich), and colleagues, randomized 334 patients slated for PCI at nine German institutions to receive a single intravenous infusion of placebo or one of two doses of revacept, 160 or 80 mg, on top of standard antithrombotic therapy prior to the procedure.
There was no difference in the primary composite endpoint of death or myocardial injury within 48 hours among the revacept 160 mg (24.4%), revacept 80 mg (25.0%), and placebo groups (23.3%; P = 0.98 for trend). A small but significant reduction of high-concentration collagen-induced platelet aggregation was seen with the higher revacept dose compared with both other study arms (P = 0.02 for trend).
No excess BARC type 2 or higher bleeding was observed within 30 days with either revacept dose compared with placebo (5.0% vs 5.9% vs 8.6%; P = 0.36).
Massberg said he had expected a greater effect of the drug on preventing myocardial injury, “but you have to consider that we were looking at a very, very low-risk population, so there was very little room for the drug to have an effect.”
Since revacept did show some efficacy in terms of platelet reactivity to collagen, Massberg said they can assume that it works in the way they had planned for it to, but many of the patients in the study were not the optimal cohort for treatment with this drug. “Troponin rises after intervention, at least in chronic coronary syndrome, are not typically triggered by thrombotic problems—mechanisms that cannot be prevented by antithrombotics to begin with,” he said. “That probably explains why we did not see [an effect here].”
A phase III trial is in the planning stages now, according to Massberg. If that shows success, he said he could see this drug being used successfully in ACS patients who need a quick-acting agent. “Typically, these patients receive potent P2Y12 inhibitors like prasugrel or ticagrelor plus aspirin but still these drugs are oral drugs,” Massberg said. “It takes some time until these drugs act.”
Additionally, he noted, “the conceptual advantage [with revacept] is that we expect lower bleeding complications with this type of drug.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Mayer K, Hein-Rothweiler R, Schüpke S, et al. Efficacy and safety of revacept, a novel lesion-directed competitive antagonist to platelet glycoprotein VI, in patients undergoing elective percutaneous coronary intervention for stable ischemic heart disease: the randomized, double-blind, placebo-controlled ISAR-PLASTER phase 2 trial. JAMA Cardiol. 2021;Epub ahead of print.
Disclosures
- ISAR-PLASTER was funded by the German Center for Cardiovascular Research, Deutsches Herzzentrum München, Federal Ministry of Education and Research, and advanceCOR GmbH (the manufacturer of revacept).
- Mayer and Massberg report no relevant conflicts of interest.





Comments