No Benefit to More-Complete Coronary Revascularization Before TAVI, Registry Shows
“I’ve been much more conservative in doing PCI,” Marco Barbanti says about how REVASC-TAVI has changed his practice.

Among patients with significant, stable coronary artery disease on a pre-TAVI workup, the completeness of myocardial revascularization does not appear to influence clinical outcomes, according to results from the REVASC-TAVI registry.
At 2 years, rates of all-cause death and a composite of death, stroke, MI, or rehospitalization for heart failure were no different between patients who had complete revascularization and those who had incomplete revascularization, researchers led by Giuliano Costa, MD (A.O.U. Policlinico “G. Rodolico – San Marco” and University of Catania, Italy), report.
The findings—presented earlier this year at EuroPCR 2022 and published recently online in Circulation: Cardiovascular Interventions—were consistent across subgroups, including those defined by age, the presence of angina or LV dysfunction, and the size of the area of myocardium at risk.
The results are not unexpected, senior author Marco Barbanti, MD (A.O.U. Policlinico “G. Rodolico – San Marco” and University of Catania), told TCTMD. The lack of difference in outcomes “was predictable considering that this is stable coronary artery disease and this is a quite old population, so the impact of coronary artery disease at 2 years is probably very mild,” he said.
Barbanti acknowledged that only a randomized controlled trial can provide a definitive answer to this question, but said that based on these registry results, it “probably may be better to have a very conservative approach” when it comes to performing myocardial revascularization around the time of TAVI in an older patient (the median age in this population was 82.6 years).
“I’ve been much more conservative in doing PCI,” he added about how REVASC-TAVI has changed his practice.
Wide Variability in Practice
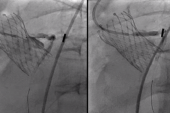
CABG at the time of SAVR has been the go-to approach in patients with both significant CAD and severe aortic stenosis for surgical candidates, but the optimal strategy in the setting of TAVI is less clear, resulting in wide variation in how concomitant coronary disease is handled across centers.
Though current guidelines recommend consideration of PCI for proximal CAD in patients undergoing TAVI, there is little randomized evidence to inform the question. The ACTIVATION trial demonstrated similar rates of death and rehospitalization at 1 year with or without PCI before TAVI, but interpretation is limited because it was stopped early, failed to demonstrate noninferiority, and excluded patients with left main disease or anginal symptoms.
To provide insights into this issue, Costa, Barbanti, and colleagues turned to the REVASC-TAVI registry, which enrolled patients who had significant, stable CAD on a pre-TAVI workup from 30 centers in Europe, North America, South America, and Japan. The current analysis included 2,025 patients, of whom 64.7% had complete revascularization and the rest had incomplete revascularization.
After propensity score matching, there were 675 matched pairs of patients (median age 82.6; 40.7% women). Overall, PCI was performed in all patients in the complete revascularization group and 43.7% of those in the incomplete revascularization. Of those who underwent PCI, the procedure was staged before or after TAVI in 72.1% and was performed at the time of TAVI in 26.3%.
The primary outcome was all-cause death at 2 years, and this did not differ between the complete and incomplete revascularization groups (21.6% vs 18.2%; HR 0.88; 95% CI 0.66-1.18). Likewise, there was no difference in the study’s co-primary outcome: all-cause death, stroke, MI, or rehospitalization for heart failure at 2 years (29.0% vs 27.1%; HR 0.97; 95% CI 0.76-1.24).
“The study raises doubts about the impact of revascularization of stable lesions in proximal segments of coronary vessels, which to date have been considered prognostically significant in this setting,” the investigators write. “Validation of functional testing to identify prognostically significant CAD and guide myocardial revascularization in TAVI setting is a priority.”
Leaning on the Heart Team
In an accompanying editorial, Homam Ibrahim, MD, and Mathew Williams, MD (both NYU Langone Health, New York, NY), say that “despite the observational nature of the study and lack of symptoms reporting upon follow-up, it adds another reminder to restrain the urge to revascularize stable CAD in patients undergoing TAVI.”
They also question whether routine invasive angiography is needed for a pre-TAVI workup, pointing to the benefits instead of obtaining a CT angiogram, which can be used to rule out the possibility of a proximal coronary occlusion and provide essential information on aortic valve anatomy.
Speaking with TCTMD, Ibrahim said he would have expected to see a lack of difference in outcomes between complete and incomplete revascularization, especially in all-comers, because of the results of the ACTIVATION trial.
He said the REVASC-TAVI results haven’t changed the approach to these patients at his center, indicating that CT has been used to avoid invasive coronary angiography and PCI in lesions unlikely to cause problems later on. “Now the aggregation of data shows that there’s really not much benefit added in treating all these lesions in either branches or mid coronary arteries,” he said.
Ibrahim stressed, however, that “this paper should not be taken to [mean] that all patients should not undergo PCI.” In their editorial, Ibrahim and Williams say “patients with left main/proximal CAD, symptomatic obstructive CAD that is refractory to medical management, and ischemic left ventricular dysfunction are examples where revascularization may be beneficial in patients undergoing TAVI.”
Importantly, Ibrahim said, the coexistence of severe aortic stenosis and obstructive CAD should be seen as a complex problem. “All of these patients should be undergoing evaluation by a heart team and getting the expertise of all the members of the heart team to evaluate the best approach,” he said.
A key thing to remember in these patients, according to Barbanti, is that even if PCI won’t be performed around the time of TAVI, coronary access should be maintained in case an intervention will be needed in the future. “Be sure that you preserve the access to the coronaries by achieving commissural alignment by implanting the right valve for the right patient,” he said.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Costa G, Pilgrim T, Amat Santos IJ, et al. Management of myocardial revascularization in patients with stable coronary artery disease undergoing transcatheter aortic valve implantation. Circ Cardiovasc Interv. 2022;15:e012417.
Ibrahim H, Williams MR. When fixing hinders, why we should sometimes fight the urge to fix. Circ Cardiovasc Interv. 2022;15:e012654.
Disclosures
- Barbanti reports being a consultant for Boston Scientifics, Edwards Lifesciences, and Medtronic.
- Costa, Ibrahim, and Williams report no relevant conflicts of interest.




Comments