Novel AI-Guided CV Risk Prediction Takes Aim at Coronary Inflammation
While promising, the technology has much to prove, including how much it really adds to standard risk prediction.
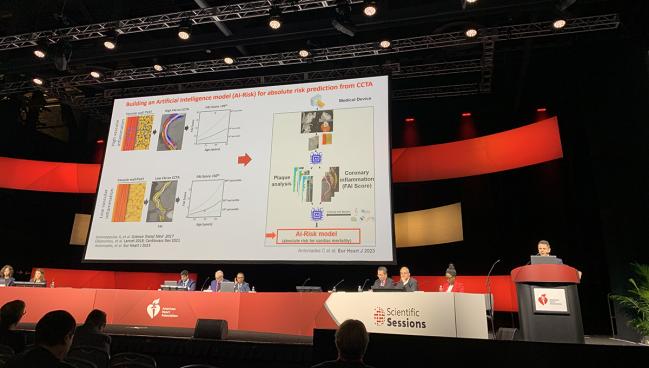
PHILADELPHIA, PA—Noninvasive imaging coupled with artificial intelligence (AI) can help characterize inflammation in fatty tissue around the coronary arteries, allowing for better prediction of future risk of cardiac events, data from the ORFAN study show.
The data, presented at the American Heart Association (AHA) 2023 Scientific Sessions this week, come at a time when the importance of inflammation’s contribution to CV risk has gained a clinical foothold, bolstered by trials such as COLCOT, CANTOS, and LoDoCo2. In June 2023, the US Food and Drug Administration approved colchicine (Lodoco; Agepha Pharma) as the first anti-inflammatory agent indicated for CV risk reduction. Moreover, there are signs that inflammation could be a more powerful risk predictor than LDL cholesterol of CV events.
“The big question is how do we identify the patients we need to treat,” said Charalambos Antoniades, MD (University of Oxford, England), during his AHA presentation.
To try to answer that question, the ORFAN investigators applied the Fat Attenuation Index (FAI) in patients undergoing coronary CT angiography (CCTA). Higher FAI is indicative of a greater degree of vascular inflammation , and prior research suggests it may be an important marker of future adverse CV events. The researchers validated the performance of FAI and an AI-assisted prognostic model to capture 8-year residual inflammatory risk via the CCTA-derived metrics, plaque analysis, and individual risk factors.
Viviany Taqueti, MD (Brigham and Women’s Hospital, Boston, MA), who was the discussant for the trial, told TCTMD that while the research is still in an early stage, it presents a “potentially intriguing tool” through which physicians may be able to leverage noninvasive imaging and squeeze more information out of it.
“The promise here is that you can start to pay attention to all of these different pieces of information and focus not just on anatomy, which has been a huge focus of invasive cardiology for the last 60 years, but start to integrate both anatomy and function,” she said, “and move beyond just looking at plaque to also considering regional, local, or even systemic inflammation and its impact on cardiovascular outcomes.”
Results Changed Management in 40%
The researchers focused on 40,091 patients (mean age 59 years; 47% female) from seven UK hospitals who underwent CCTA. Of these, 18% had obstructive CAD. MACE occurred in 20.1% of those with obstructive CAD and 9.5% of those with nonobstructive CAD (P < 0.001).
The FAI with AI guidance was evaluated in a nested cohort of 3,393 consecutive ORFAN patients with follow-up data out to a median of 7.7 years. Those with FAI scores in the left anterior descending (LAD) artery above the 75th percentile had a greater risk of MACE than those below the 25th percentile (HR 6.75; 9%% CI 5.21-8.78) and a greater risk of cardiac mortality (HR 20.20; 95% CI 11.49-35.53). Risk prediction was similar for all vessels, independent of risk factors and other CCTA-derived measures.
Even in those with nonobstructive CAD, having a high FAI was associated with greater risk of MACE (HR 4.77; 95% CI 3.40-6.69) and cardiac mortality (HR 10.49; 95% CI 5.25-20.95) than having lower FAI levels.
Importantly, the AI-guided risk prediction resulted in reclassification of 30% of patients to a higher risk category and 10% to a lower risk category, Antonaides said. Changes in management initiated by clinicians receiving the results included statin initiation in 24%, statin dose-intensification in 13%, and additional or further treatments, including colchicine, in 8%.
“This model of AI risk assessment may transform risk stratification and management of patients undergoing routine CCTA,” Antonaides concluded.
Future Considerations
The nested study results presented here are only a small portion of the CCTA assessment with AI guidance that the ORFAN investigators plan to assess. The ultimate goal is to validate the prediction model in 250,000 scans.
In her discussion, Taqueti noted that the generalizability of the results is limited since the cohort is largely white and low risk. To TCTMD, she said another unknown is how patients were selected for coronary CTA. According to the ORFAN investigators, the participants have all been asked by their clinical care team to undergo a cardiac CT scan.
“The other thing is that the data they presented are mostly unadjusted. Once you start to adjust for existing variables like diabetes and previous heart disease and maybe low ejection fraction, you might see an attenuation of the hazard,” she noted. “There's a lot of interesting potential, [but] the real proof will be in the details of the data and scrutinizing the data carefully.”
Also potentially important, Taqueti said, is understanding whether the FAI correlates with other known biomarkers like high-sensitivity C-reactive protein and interleukin-6, which are known to be elevated in those with residual inflammatory risk. Understanding the scientific mechanisms underpinning the elevated risk also is important.
“Is it endothelial dysfunction, is it vasomotor dysfunction, is it microvascular dysfunction, or is it something else?” she asked. “I think that bears additional scrutiny. If you look closely at the curves, they actually separate very early on. So again, that reflects that there's probably some baseline differences that haven’t been fully adjusted for in this analysis. We really need to understand how much of this risk is specifically attributable to this novel index, which obviously would be exciting, versus what the AI is considering for all of the other factors that we would be able to pick up anyway.”
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Antoniades C. Novel AI technology to improve risk stratification of patients without obstructive coronary artery disease undergoing CCTA: the Oxford risk factors and non-invasive imaging (ORFAN) study. Presented at: AHA 2023. November 13, 2023. Philadelphia, PA.
Disclosures
- ORFAN is supported with funding from the Oxford Biomedical research Centre, The British Heart Foundation, Innovate UK, the National Consortium for Intelligent Medical Imaging and the European Commission.
- Antoniades reports research grants from Sanofi and NovoNordisk; consulting for Mitsubishi-Tanabe, Silence Therapeutics, and Caristo; honoraria from Amarin and Covance; and research contracts from MedImmune/AstraZeneca.
- Taqueti reports no relevant conflicts of interest.





Comments