Pandemic Blamed for Loss of BP Control That Has Not Fully Rebounded
The phenomenon is not without precedent, with many CVD risk factors increasing following natural disasters, says one expert.
The COVID-19 pandemic resulted in substantial disruptions in optimal blood pressure control among hypertensive patients in the United States, according to the large BP Track study.
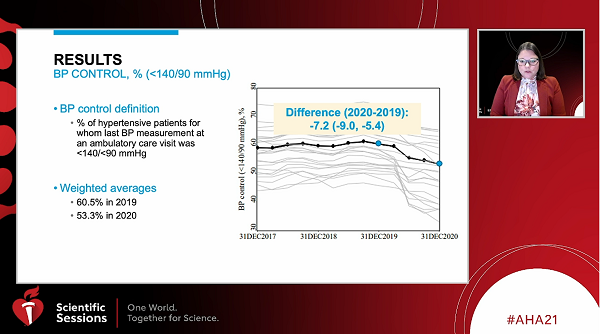
“The weighted average of blood pressure control was 60.5% in 2019, and it dropped 7.2% to 53.3% in 2020,” said Alanna M. Chamberlain, PhD (Mayo Clinic, Rochester, MN), in a late-breaking science session last weekend at the virtual American Heart Association (AHA) 2021 Scientific Sessions. The data also show a decline in timely follow-up visits compared with 2019.
While the study did not include data for 2021, Chamberlain said it was clear by the end of 2020 that there had been little rebound to prepandemic levels in most of BP metrics examined. “Importantly, continuous surveillance is needed to determine whether this decline in blood pressure control during the pandemic will result in future cardiovascular death,” she added. BP Track was already ongoing prior to the pandemic, Chamberlain noted, which allowed for timely capture of a variety of metrics from nearly 1.8 million patients with a concurrent or prior diagnosis of hypertension.
Session co-moderator Keith Ferdinand, MD (Tulane University, New Orleans, LA), said the phenomenon is not without precedent, noting that “after natural disasters, we've seen this rise in uncontrolled risk factors. It's then followed by cardiovascular disease. So, you want to continue to look at these patients’ outcomes.” One important next step will be to analyze data on telehealth follow-up visits “to see whether or not having a telehealth visit would blunt the difficulty in maintaining blood pressure control,” said Ferdinand.
BP Track Findings
Data for the study came from 24 healthcare systems in the United States participating in the PCORnet Blood Pressure Control Laboratory Surveillance System (BP Track). The number of patients for whom multiple BP metrics in the year before the pandemic through 2020 were available was 1,770,547. BP control was defined in the study as the percentage of hypertensive patients whose most recent ambulatory BP was < 140/90 mm Hg. Timely follow-up was defined as the percentage who had a subsequent visit within 4 weeks of an ambulatory pressure reading > 140/90 mm Hg.
The percentage of patients with previously uncontrolled BP who achieved either a reduction of at least 10 mm Hg, or a systolic pressure < 140 mm Hg, was about 6% lower in 2020 compared with 2019. Looking at the percentage of patients with uncontrolled BP who had timely follow-up showed a similar decline from 36.7% in 2019 to 31.7% in 2020. Chamberlain said a dramatic drop in these visits occurred early on in the pandemic and was accompanied by a later increase.
BP Track also looked at BP control to < 130/80 mm Hg to align with the 2017 AHA/American College of Cardiology hypertension guidelines. The downward trend from 2019 to 2020 was similar, although Chamberlain pointed out that even the prepandemic rate of control at this tighter level was only 30%.
Another metric measured in BP Track was medication intensification, which was defined as the percent of visits by individuals with uncontrolled hypertension that included prescription of a different class of blood pressure medication. This proved to be one of the few areas that was not negatively affected by the pandemic. New medication prescription increased slightly from 10.8% in 2019 to 11.7% In 2020. Finally, the researchers looked at trends by race and ethnic groups, finding consistently lower BP control in non-Hispanic Black patients compared with all other groups despite a somewhat higher rate of timely repeat visits for uncontrolled hypertension.
I'm hopeful that if we were able to extend this to June or July 2021, that we may see that things were at least starting to rebound slightly. Jordana Cohen
Commenting for TCTMD, Jordana B. Cohen, MD (University of Pennsylvania, Philadelphia), said even with the limitations of the data, particularly not having patient-level information to confirm that the patients in 2020 and 2019 were similar, she was surprised the results weren’t worse.
“This is a very broad view of what we all suspected,” Cohen said. Ending the study just as vaccinations were beginning to take hold in the United States, she added, makes it hard to know what we can expect for 2021.
“A lot of us are seeing our clinics getting much busier, with people coming back in to be seen,” she observed. “I don't think that we are by any means back to normal now, but I'm hopeful that if we were able to extend this to June or July 2021, that we may see that things were at least starting to rebound slightly.”
Cohen agreed with Ferdinand that the contribution of telehealth visits should be further examined.
“I actually think telehealth is part of why the numbers weren't worse than they were,” she said. “My patient attendance at visits when I did telehealth during the pandemic was about 100%, whereas right now, about one-quarter of people don't come in for office visits. Telehealth is an amazing way to remove barriers to care.” Particularly with regard to BP, she said, those visits give physicians an opportunity to train patients how to take their measurements at home properly.
“It also puts some of the ball in their court, where they have a sense of ownership and control over their blood pressure,” Cohen added.
Chamberlain said telehealth visits are captured by most health systems in common data models, so it may be possible to separate out telehealth visits versus other visits for future analyses similar to BP Track.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Chamberlain AM. Disruption in blood pressure control with the COVID-19 pandemic: a study of 24 US health systems in the PCORnet blood pressure control laboratory. Presented at: AHA 2021. November 13, 2021.
Disclosures
- Chamberlain reports a research grant from EpidStrategies.
- Cohen reports no relevant conflicts of interest.




Comments