PCI Comparable to CABG in Left Main Coronary Disease: Meta-analysis
The study reaffirms what was observed in the large EXCEL trial, suggesting PCI is an acceptable option in left main disease, say researchers.
A new meta-analysis, one that includes the EXCEL and NOBLE trials, provides further support for PCI in patients with unprotected left main coronary artery disease.
Across six randomized clinical trials, all-cause mortality was equivalent between patients treated with PCI and those undergoing coronary artery bypass graft surgery in both short- and long-term follow-up. While PCI was associated with an early safety benefit, CABG surgery was associated with a lower risk of major adverse cardiovascular and cerebrovascular events over long-term follow-up, a finding driven by a higher risk of repeat revascularization in the PCI-treated patients.
Jari Laukkanen, MD, PhD (University of Eastern Finland, Kuopio), who led the study, said there are “philosophical differences” between proponents of PCI and CABG, but that the overall data suggest PCI is an acceptable treatment alternative to surgery in patients with left main coronary artery disease, particularly since PCI is associated with shorter hospital stays and better quality of life in the short term.
Laukkanen noted that PCI is performed frequently in Finland for the treatment of left main disease and that the decision is based on discussions with the heart team to determine appropriately suitable patients.
Of the studies in their meta-analysis, he told TCTMD, only one trial has follow-up to 10 years, though. In the others, follow-up ranges from 1 to 5 years. For this reason, longer follow-up will be needed to determine the relative merits of PCI versus CABG, said Laukkanen.
Still, Laukkanen said that if the coronary anatomy is suitable, PCI provides yet another treatment option for patients with left main coronary stenosis. Given the evidence from clinical trials, as well as the frequently increased use of PCI in clinical practice, the European guidelines should be updated to strengthen the support for PCI in left main disease, he urged.
In the US and European guidelines, CABG is a class I recommendation for the treatment of unprotected left main coronary artery disease. In Europe, PCI is a class I recommendation for low-risk patients but class IIa and III for intermediate- and higher-risk patients, respectively. In the United States, PCI is class IIa or IIb recommendation—meaning it is or may be reasonable—for low-to-intermediate-risk patients.
Early Safety Advantage With PCI
The meta-analysis, which was published online in Open Heart, includes LE MANS, SYNTAX, PRECOMBAT, EXCEL, NOBLE, and a 201-patient German study with 1-year follow-up.
Regarding all-cause mortality, there was no significant difference between patients treated with PCI versus CABG at 30 days, 1 year, and 3 years and beyond. Stroke rates were significantly lower at 30 days and 1 year in the PCI-treated patients, although PCI was associated with increased coronary revascularization at 3 to 5 years of follow-up. There were no significant differences in the risk of MACCE at 30 days or 1 year, but PCI was associated with a higher MACCE risk in follow-up at 3 years and beyond (HR 1.27; 95% CI 1.12-1.44). The increased MACCE rate was driven by higher rates of coronary revascularization (HR 1.70; 95% CI 1.42-2.05).
Overall, there was no long-term difference in the risk of death, stroke, or MI between patients treated with PCI and those treated surgically, but the 30-day results favored PCI.
Commenting on the analysis for TCTMD, Gregg Stone, MD (NewYork-Presbyterian/Columbia University Medical Center, New York, NY), the lead investigator of EXCEL, said the meta-analysis demonstrates an early safety advantage for PCI. But later catch-up reveals the two procedures to be comparable with respect to the important composite endpoint of death, stroke, or MI, he added.
“I do think these results are very consistent with the EXCEL trial but are important because they extend those results to a much larger group of patients treated with different types of drug-eluting stents and different bypass procedures,” said Stone.
David Kandzari, MD (Piedmont Heart Institute, Atlanta, GA), told TCTMD that the meta-analysis is one of several comparing left main PCI versus CABG, “all of which show very consistent results.” Meta-analyses, in general, offer insight into outcomes that can be expected in clinical practice and help inform discussions with the heart team and with the patient, said Kandzari.
“It is important to realize, too, that these are often very selected patients enrolled in clinical trials,” he said. “However, in the EXCEL [trial], these patients represent the majority of those for whom left main PCI is considered.”
He added that while meta-analyses typically focus on traditional clinical events, comparative studies that focus on quality of life by weighing the relevance and impact of stroke and repeat revascularization on health status have shown PCI and CABG to be even more comparable. Improvements in angina symptoms and quality of life expectedly exceed surgery during the period of early recovery and are sustained and similar to surgery through 3 years, said Kandzari.
“These considerations are fundamental in routine clinical practice when patients and their families participate in shared decision-making,” he said.
In terms of the higher rate of repeat revascularization with CABG, Stone pointed out that surgery comes with its own drawbacks, such as new-onset atrial fibrillation, operative complications, lengthened hospital stay, and worse quality of life in early recovery. When treated with contemporary drug-eluting stents, approximately one in 20 patients will need to undergo repeat revascularization, said Stone.
Regarding the follow-up period, Stone said that given the age of most patients with coronary artery disease—the average age of patients in EXCEL and NOBLE was 65 years—the 3- to 5-year horizon is very important. For this reason, he believes the data are sufficient to change the guidelines to strengthen the recommendation for PCI in the treatment of left main coronary disease.
“Certainly, longer-term follow-up would be very important to see if any major differences emerge between PCI and CABG after revascularization, which would be especially relevant to younger patients,” said Stone.
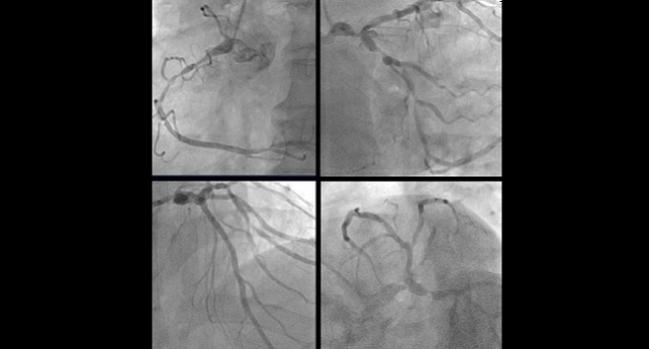
Photo Credit: Adapted from Ahn J-M. Case #1 Conclusion: A Diabetic Patient With Left Main Disease. How We Treated. Presented at: TCT 2017. November 1, 2017. Denver, CO.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Laukkanen JA, Kunutsor SK, Niemela M, et al. All-cause mortality and major cardiovascular outcomes comparing percutaneous coronary angioplasty versus coronary artery bypass grafting in the treatment of unprotected left main stenosis: a meta-analysis of short-term and long-term randomized trials. Open Heart. 2017;4:e000638.
Disclosures
- Laukkanen reports no relevant conflicts of interest.
- Stone reports consulting for Reva Medical.
- Kandzari reports grant support from Abbott Vascular, Medtronic, Orbus Neich; consulting/honoraria/speaker’s bureau for St. Jude Medical, Boston Scientific, Medtronic, and Micell.


Comments