PRECEPT Provides Support for Ablation of Symptomatic, Persistent A-fib
Ablation using a contact force-sensing radiofrequency catheter was safe and appeared to be effective in the single-arm study.
Ablation of drug-refractory, symptomatic, persistent atrial fibrillation is safe and effective when using a contact force-sensing radiofrequency catheter, findings of the single-arm PRECEPT study suggest.
The rate of primary safety events was 3.8%, coming in below the performance goal of 16.0%, and the rate of the primary effectiveness endpoint was 61.7% at 15 months, exceeding the performance goal of 40.0%, Moussa Mansour, MD (Massachusetts General Hospital, Boston), reported at the Heart Rhythm Society (HRS) 2020 Scientific Sessions, which took place online as a “virtual” meeting last week. The results were published simultaneously online in JACC: Clinical Electrophysiology.
Moreover, clinical success—defined as freedom from documented symptomatic atrial fibrillation, flutter, or tachycardia recurrence—at 15 months was 80.4%. “This may be a useful success rate to talk to patients about rather than the 30-seconds recurrence rate, which may not be a good representation for clinical outcome in patients with persistent atrial fibrillation,” Mansour said.
Commenting for TCTMD, Fred Kusumoto, MD (Mayo Clinic, Jacksonville, FL), president-elect of the HRS, called PRECEPT an important trial that is theoretically going to lead to the first ablation catheter approved by the US Food and Drug Administration for persistent—as opposed to paroxysmal—A-fib. The study indicates that “with the current approaches, catheter ablation in patients with persistent atrial fibrillation appears to be safe,” he said.
An effectiveness rate of about 60% is good, he said, adding the caveat that additional detail on the types of patients included in the study will be important. “We don’t exactly know the clinical characteristics of these patients,” Kusumoto said. Patients with long-standing persistent A-fib have historically been difficult to treat with catheter ablation, so if “it turns out these were the patients studied, well then this will be quite a remarkable study,” he added.
With the current approaches, catheter ablation in patients with persistent atrial fibrillation appears to be safe. Fred Kusumoto
Kusumoto highlighted the fact that PRECEPT also showed reductions in the utilization of healthcare resources, including cardioversion and antiarrhythmic drugs, as well as gains in quality of life. “That obviously is an important thing as we think about how best to treat patients and the improvement in quality of life in these patients,” he said, noting that those results are consistent with prior studies like the CABANA trial. “It is good that the study has been confirmatory of these other results suggesting that catheter ablation, even in these very ill patients with significant atrial fibrillation burden, is generally a good thing in selected patients.”
PRECEPT
Mansour noted that even though the safety and effectiveness of catheter ablation for paroxysmal A-fib has been established, there are limited data on ablation outcomes in persistent A-fib. No catheters are currently FDA-approved for persistent A-fib, although off-label use is common in the United States.
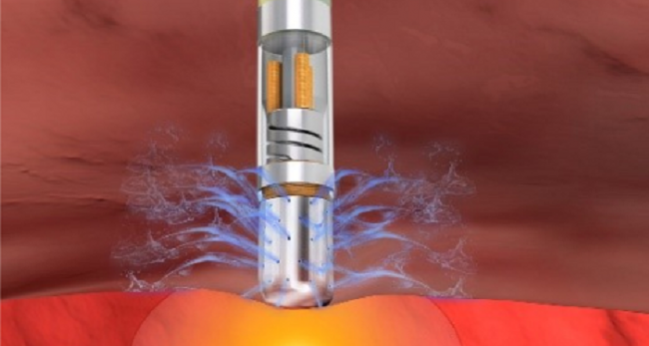
PRECEPT is a prospective, single-arm, investigational device exemption (IDE) study conducted at 27 sites in the US and Canada designed to evaluate ablation of persistent A-fib using the Thermacool Smartouch SF contact force-sensing radiofrequency catheter guided by the Carto Visitag module (Biosense Webster). Patients had symptomatic persistent A-fib along with nonresponse or intolerance to at least one class I/III antiarrhythmic drug. Most (about 70%) were men, and the mean age was 65. On average, the duration of symptomatic persistent A-fib was about 16 months, with participants having failed a mean of 1.3 antiarrhythmic drugs at baseline.
The primary safety endpoint encompassed adverse events occurring within 7 days of initial or repeat ablation procedures. Of the 344 patients who had a catheter inserted and were included in the analysis, 3.8% had a safety event, most commonly cardiac tamponade (five cases), major vascular access complications/bleeding (three cases), and pericarditis (two cases). Eleven of the 14 events resolved without sequelae, Mansour reported.
Primary effectiveness was evaluated using a composite consisting of freedom from documented recurrence of atrial fibrillation, flutter, or tachycardia; acute procedural failure; use of nonstudy catheters; repeat ablations; use of a new or higher dose of antiarrhythmic drug; and surgical ablation. Of the 333 patients included in this analysis, the Kaplan-Meier estimated rate at 15 months was 61.7%.
From baseline to 15 months, use of cardioversion dropped from 62.0% to 10.7% and use of class I/III antiarrhythmics fell from 97.0% to 24.7% (post hoc P < 0.001 for both). At the end of the study, freedom from repeat ablation was 86.1% and freedom from CV hospitalization was 84.2%.
Moreover, 81.0% of patients were asymptomatic according to the Canadian Cardiovascular Society Severity in Atrial Fibrillation scale at 15 months, compared with just 0.7% at baseline. There was also an improvement in Atrial Fibrillation Effect on Quality of Life scores.
Ablation Safe, but Is It Effective?
Providing commentary after Mansour’s presentation, Sana Al-Khatib, MD (Duke University Medical Center, Durham, NC), said there is an important need to improve ablation in patients with long-standing persistent A-fib. One way is to use better catheters, she said, adding that “the safety and efficacy profiles of the studied catheter are indeed encouraging.”
Al-Khatib said there are still some outstanding questions, among them how the catheter performs in patients with more remodeling and more advanced structural heart disease, whether the effects are durable, and whether treatment is cost-effective.
Another issue to keep in mind, she commented, is that PRECEPT was conducted by experienced operators. “It would be good to get more data on this catheter, perhaps in real-world settings, and to see if these results can be replicated by other groups,” she said.
Eric Prystowsky, MD (Ascension Medical Group, Indianapolis, IN), also commenting after presentation, said he wants to see additional data as well.
“I’m okay with” the 3.8% complication rate, he said, because “that’s within the typical accepted complication rates we see in these types of patients.” But he indicated that he would need a closer look at the efficacy data before drawing any conclusions.
“I’m not overly impressed to be frank,” Prystowsky said. “There are more recent data looking at cryoablation in patients with persistent A-fib just with [pulmonary vein isolation] and they come up with pretty good results. So I think the true test of this catheter is to compare it to something else and then we’ll find out the efficacy. But as far as safety, I think the authors have shown me that it’s fine.”
Photo Credit: Biosense Webster Inc.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Mansour M, Calkins H, Osorio J, et al. Persistent atrial fibrillation ablation with contact force sensing catheter: the prospective multicenter PRECEPT trial. J Am Coll Cardiol EP. 2020;Epub ahead of print.
Disclosures
- PRECEPT is funded by Biosense Webster.
- Mansour reports having served as a consultant for Biosense Webster, Abbott, Medtronic, Boston Scientific, Janssen, Philips, Novartis, and Sentre Heart; having received research grants from Biosense Webster, Abbott, Boston Scientific, Medtronic, Pfizer, and Boehringer Ingelheim; and having an equity interest in EPD Solutions, NewPace Ltd, and Affera.
- Kusumoto reports no relevant conflicts of interest.


Comments