PROSPECT MONSTER: Real-World Data Confirm Low-Dose DCB Efficacy in PAD
As in the COMPARE trial, the data show sustained treatment benefit to 1 year with low- and high-dose DCBs.
LEIPZIG, Germany—Using second-generation low-dose paclitaxel drug-coated balloons (DCBs) in a complex patient population with femoropopliteal artery disease results in similar primary patency and freedom from reintervention out to 1 year compared with high-dose DCBs, according to a real-world analysis.
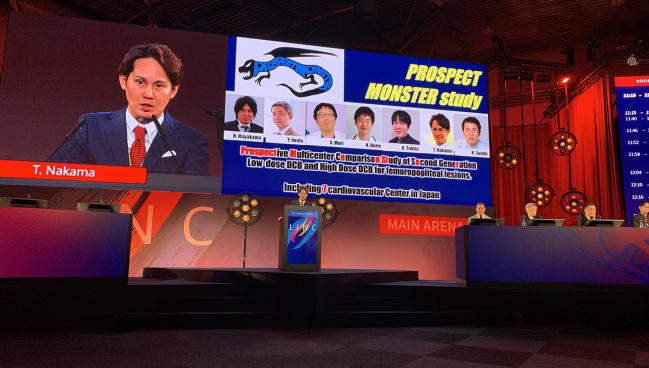
PROSPECT MONSTER was designed to address the efficacy of second-generation low-dose DCBs in light of recent data from the POPCORN registry of over 3,100 de novo or restenotic femoropopliteal lesions suggesting that use of a first-generation low-dose DCB (Lutonix; Bard), versus a high-dose DCB, was one of several factors independently associated with 1-year restenosis (HR 1.97; 95% CI 1.61-2.41), said Tatsuya Nakama, MD (Tokyo Bay Urayasu Ichikawa Medical Center, Chiba, Japan), in his presentation here at LINC 2023.
The only other head-to-head comparison of high- versus low-dose DCBs in the treatment of femoropopliteal artery disease comes from the randomized European COMPARE trial. No significant difference in primary patency or rates of all-cause mortality were seen at 2 years in a wide range of lesion lengths in COMPARE patients treated with In.Pact DCB (Medtronic), which has a paclitaxel dose on the balloon of 3.5 µ/mm2, or the second-generation Ranger DCB (Boston Scientific), which has a dose of just 2 µ/mm2.
“However, there is no real-world comparison data about second-generation low-dose DCB and high-dose DCB,” Nakama noted.
As he showed here, there was no difference in primary patency at 12 months between the high-dose and low-dose DCBs (81.6% vs 87.4%; P = 0.66). In the randomized COMPARE trial, by contrast, the 1-year primary patency rates were 88.7% and 87.7%, respectively (log rank P = 0.96).
The exact amount of drug needed to obtain antirestenotic efficacy in peripheral lesions is not clear, but interest in using lower doses of paclitaxel has surged in recent years due to concerns raised by a 2018 meta-analysis suggesting higher long-term mortality rates among PAD patients treated with paclitaxel DCBs and stents compared with plain old balloon angioplasty (POBA). At the time, some speculated that higher doses might be responsible for toxicity and deaths in the paclitaxel-treated patients, but that theory has been largely debunked by multiple studies, including the SAFE-PAD analysis and an independent, patient-level data analysis of paclitaxel-containing devices conducted by VIVA showing no dose-response relationship to long-term mortality.
No Difference in Freedom From CD-TLR
For PROSPECT MONSTER, Nakama and colleagues looked at 1-year outcomes for 370 patients (mean age 74 years) treated with the second-generation low-dose DCB and 211 treated with the high-dose DCB at seven centers in Japan from 2021-2022. Patients were propensity-score matched to eliminate differences in baseline characteristics, resulting in 359 in the low-dose group and 167 in the high-dose group.
Nearly three-quarters of patients were smokers and had diabetes. About one-third had CKD without dialysis and another one-third had CKD and were on dialysis. Approximately 40% had chronic limb-threatening ischemia (CLTI; Rutherford category 4 or 5), and one-third of lesions had popliteal involvement. The mean reference vessel diameter was 5.4 mm, and the mean lesion length was 184 mm in the low-dose group and 176 mm in the high-dose group, which Nakata noted was longer than the mean length of lesions in the COMPARE trial. Additionally, approximately one-quarter of all patients had a chronic total occlusion and 45% had peripheral artery calcification scoring system (PACSS) grade 3 or 4 lesions.
In addition to the lack of significant difference in the primary endpoint between the high-dose and low-dose DCB in PROSPECT MONSTER, there also was no gap in freedom from clinically driven TLR at 1 year (90.2% vs 93.2%; P = 0.80) or differences in rates of impaired flow, bailout stenting, or perioperative complications. Nakama noted that due to the Japanese healthcare system not reimbursing for bailout stenting, its use was extremely low in comparison to most of the DCB literature—just 3% in the low-dose group and less than 2% in the high-dose group.
In an interaction analysis, patients with diabetes had a lower risk of restenosis with the high-dose DCB compared with the low-dose DCB (P = 0.031 for interaction), as did those with lesions with a reference vessel diameter less than 6 mm (P = 0.036 for interaction).
Bailout Stenting Overused?
Session moderator Ramon Varcoe, MBBS, PhD (Prince of Wales Hospital, Sydney, Australia), said he was struck by the high primary patency rates despite the extremely low use of bailout stenting, adding that it begs the question of whether “the rest of the world is overusing bailout stenting” in femoropopliteal revascularizations.
Nakama said Japanese operators tend to view even type C dissections as essentially benign and believe that the literature supports that opinion.
“The fact that the 1-year endpoints didn't suffer when they didn't bailout stent, even if they had a meaningful number of type C dissections, speaks to their approach,” said Eric A. Secemsky, MD (Beth Israel Deaconess Medical Center, Boston, MA), who commented on the findings for TCTMD.
“We do a lot of guesswork with dissections, and typically it's based on impairment in flow and oculostenotic reflex and whether you feel comfortable walking away from it or not,” he added.
While there are angiogram-based dissection criteria that have primarily been adapted from the coronary literature ,“we need some better evidence in terms of algorithms for treating dissections and in terms of what patency looks like long term. We probably do put more stents in than we need to help us get over the bump on the short-term side,” Secemsky said. “If you have to put in a scaffold to cover a dissection, maybe you didn't vessel prep or balloon enough. Maybe you have a risk of that stent restenosing and then you potentially create more problems down the line.”
“[PROSPECT MONSTER] tells us [that] if we do that, we can safely use second-generation low-dose DCB in CLTI patients and the clinical outcomes are almost the same as with the high-dose DCB,” he added.
Unlike the United States and much of Europe, Japan is known for high rates of IVUS use in peripheral interventions, with Nakama noting that it was used in nearly 70% of all cases in PROSPECT MONSTER and may have been another contributor to the good outcomes despite virtually no bailout stenting.
Secemsky, who authored a consensus document last year on the emerging use of IVUS in peripheral interventions, said it’s important to continue to gather information on how it can impact outcomes. One single-center study suggested that 1-year risk of restenosis is lower with the use of IVUS to guide therapy, presumably because the imaging boosts vessel sizing accuracy, but larger data sets are lacking, he added.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Nakama T. Second-generation low-dose drug-coated balloon vs high-dose drug-coated balloon for symptomatic femoropopliteal artery disease: the result from the PROSPECT-MONSTER study. Presented at: LINC 2023. June 8, 2023. Leipzig, Germany.
Disclosures
- Nakama reports consulting for BD, Boston Scientific, Cook, Medtronic, Century Medical, Cordis, Nipro, and OrbusNeich; and honorarium from Abbott Vascular, Asahi, Boston Scientific, BD, Cook, Cordis, Kaneka, Nipro, Medtronic, OrbusNeich, and Terumo.
- Secemsky reports consulting/Speakers Bureau/advisory board for Abbott, Bayer, BD, Boston Scientific, Cook, CSI, Endovascular Engineering, Inari, Janssen, Medtronic, Philips, and VentureMed; and grants to his institution from AstraZeneca, BD, Boston Scientific, Cook, CSI, Laminate Medical, Medtronic, and Philips.





Comments