Pulsed-Field Ablation Equals, and May Top, Cryoablation for Paroxysmal AF
The SINGLE SHOT CHAMPION study increases momentum for PFA as a first-line option for pulmonary vein isolation, say experts.
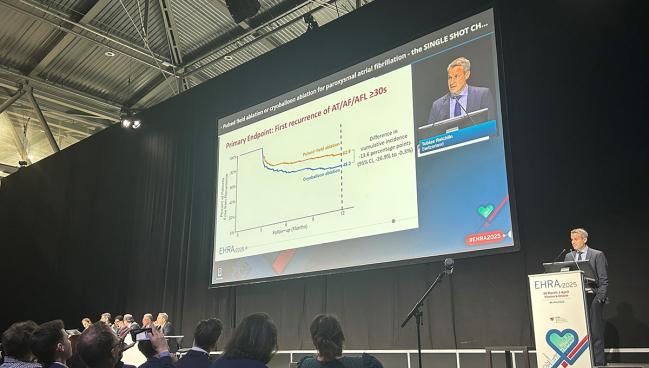
Excluding a 3-month blanking period, the rate of a first recurrence of an atrial tachyarrhythmia lasting at least 30 seconds at 1 year was 37.1% in patients treated with pulsed-field ablation (PFA) and 50.7% in those treated with the cryoballoon (P < 0.001 for noninferiority; P = 0.046 for superiority).
“The sample size of our trial is modest and the superiority test of borderline statistical significance, so the superior efficacy of PFA should be further investigated in larger outcome trials,” Tobias Reichlin, MD (Inselspital – University Hospital Bern, Switzerland), reported here at the European Heart Rhythm Association Congress 2025.
The results were published simultaneously online in the New England Journal of Medicine.
Luigi Di Biase, MD, PhD (Albert Einstein College of Medicine at Montefiore Hospital, Bronx, NY), who commented on the results for TCTMD, said the findings are exciting news for PFA.
“For me, the message is that PFA is a better energy source to perform PVI” than the cryoballoon, he said, adding that there remains some question about how it will compare to radiofrequency ablation in a one-on-one trial. It’s likely that PFA will be at least noninferior to radiofrequency ablation as well, and with gaining operator experience with the new modality, “I think over time, PFA will probably completely replace thermal energy,” Di Biase said.
SINGLE SHOT CHAMPION Trial
PFA has emerged in recent years as an alternative to thermal modalities, including radiofrequency and cryoablation. It’s touted as a safer option because its mechanism of action—electroporation—is more specific for myocardial tissue, reducing the likelihood of damage to surrounding structures like the esophagus, pulmonary vein, and phrenic nerve.
The ADVENT trial previously showed that PFA with Farapulse had noninferior efficacy and safety, accompanied by faster procedural times, compared with either radiofrequency or cryoballoon ablation in patients with paroxysmal AF. Recurrence of atrial tachyarrhythmia was similar across ablation modalities, consistent with observational studies. None of those studies, however, employed continuous rhythm monitoring to detect recurrences and measure AF burden.
SINGLE SHOT CHAMPION, conducted at two high-volume tertiary care centers in Switzerland with experienced operators, included 210 patients (mean age 64 years; 28% women) with symptomatic paroxysmal AF randomized to PFA or cryoablation (Arctic Front; Medtronic) for a first pulmonary vein isolation. All received an implantable cardiac monitor (Reveal LinQ; Medtronic) to detect atrial tachyarrhythmias after ablation.
Repeat ablation was not allowed during the 3-month blanking period after the procedures. Antiarrhythmic drugs could be used during that time but had to be stopped for the rest of follow-up.
Mean procedure duration was shorter with PFA versus cryoablation (55 vs 73 minutes), with a similar mean fluoroscopy time (14.6 vs 15.1 minutes). Mean high-sensitivity troponin levels were higher after PFA (1,920 vs 1,114 ng/L).
The difference in the incidence of a first recurrence of an atrial tachyarrhythmia from 91 to 365 days was -13.6% (95% CI -26.9% to -0.3%), favoring PFA over cryoablation. That met criteria for noninferiority, with the upper limit of the confidence interval falling below 20%. The difference in atrial arrhythmia recurrence when considering the entirety of the first year after ablation was -18.2%.
“We could see that in the first 90 days, the difference between the two modalities was most striking, and I think this is important because it means that the difference in the mechanisms of cardiac injury during ablation translates [into] differences in the pattern of cardiac recovery in the month following ablation,” Reichlin said.
The difference in the mechanisms of cardiac injury during ablation translates [into] differences in the pattern of cardiac recovery in the month following ablation. Tobias Reichlin
Mean atrial arrhythmia burden was significantly lower in the PFA versus cryoablation arm during the blanking period (-2.4% difference), but the advantage was smaller (-0.5%) and no longer significant from 91 to 365 days.
The main safety endpoint was a composite of procedure-related complications within 30 days, and there were few events: one patient in the PFA arm had a minor stroke, whereas two patients treated with the cryoballoon developed cardiac tamponade requiring drainage. One patient in the PFA group died of cancer 11 months after ablation.
Hospitalization or emergency department visits for recurrence of atrial arrhythmia occurred in fewer patients treated with PFA versus cryoablation (two versus eight), but the difference wasn’t significant. Repeat ablations after the blanking period were numerically, but not significantly, higher in the PFA arm (15.2% vs 9.5%).
Quality of life—measured using EQ-5D-5L composite score and a visual analog scale—was similar in the two arms of the trial at 3 and 12 months.
Moving the Needle Toward PFA
Prashanthan Sanders, MBBS, PhD (University of Adelaide and Royal Adelaide Hospital, Australia), the discussant following the presentation, highlighted key differences between SINGLE SHOT CHAMPION and the prior ADVENT trial. The latter was larger, involved a greater number of centers, compared PFA with both radiofrequency and cryoballoon ablation, and used only intermittent monitoring for recurrent arrhythmias.
Importantly, freedom from recurrent arrhythmias at 1 year was less in SINGLE SHOT CHAMPION, “perhaps due to the continuous monitoring that we see,” Sanders said.
He cautioned, however, against reading too much into the superiority analysis. “The superiority criteria only just met significance, and it would actually only take a handful of patients to move either way for this not to reach significance, and this is really hypothesis-generating in terms of how we should interpret this.”
The superiority criteria only just met significance, and it would actually only take a handful of patients to move either way for this not to reach significance. Prashanthan Sanders
Sanders also highlighted safety, noting that serious adverse events in SINGLE SHOT CHAMPION were few in number, “but in percentage, significant.” Regarding the single stroke in the PFA group, he said: “In light of the silent cerebral lesions described in ADVENT, one needs to be cognizant, as this technology moves towards becoming more first-line, that this is something our field needs to be watching out for.”
Another issue raised by Sanders was the higher number of redo ablations performed in SINGLE SHOT CHAMPION than in ADVENT, which might be due to the closer monitoring of arrhythmias during follow-up. “One of the dangers here is, although we are keen to use implantable monitors, this may actually drive us to do more procedures, and we need to be cognizant of this in future study designs,” he said.
Despite these and other issues, however, the trial “really shifts the needle towards offering PFA as more of a first-line treatment,” Sanders said.
Reichlin acknowledged some limitations of the study, including the use of a single PFA system, meaning the results may not apply to other technologies; the lack of information on AF burden before ablation; and uncertain generalizability stemming from the fact that the trial was conducted by experienced operators in just two high-volume centers.
Di Biase said future trials should ensure that AF burden is measured both before and after ablation so it can be used as a measure of success/failure instead of using detection of short episodes of AF.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Reichlin T, Kueffer T, Badertscher P, et al. Pulsed field or cryoballoon ablation for paroxysmal atrial fibrillation. N Engl J Med. 2025;Epub ahead of print.
Disclosures
- The trial was supported by the Inselspital (University Hospital Bern) and the University Hospital Basel, as well as by an unrestricted research grant from Boston Scientific, which was used to cover the cost of the implantable cardiac monitors.
- Reichlin reports receiving grants/contracts from Abbott, Biosense Webster, Biotronik, Boston Scientific, and Medtronic and consulting for Abbott, Bayer, Biosense Webster, Biotronik, Boston Scientific, Bristol Myers Squibb, Medtronic, and Pfizer.
- Di Biase reports being a consultant for Stereotaxis, Biosense Webster, Boston Scientific, Abbott Medical, and Rhythm Management; and having received speaker honoraria/travel support from Biotronik, Medtronic, AtriCure, Bristol Myers Squibb, and Pfizer.





Comments