RAISE: Reteplase May Be Another Option for Stroke Thrombolysis
The agent improved functional outcomes over alteplase, but further validation is needed, one expert says.

Reteplase appears to be another safe and effective thrombolytic option for the treatment of acute ischemic stroke, according to results from the randomized RAISE trial.
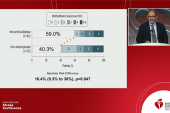
When given within the first 4.5 hours after stroke onset, reteplase led to a higher rate of excellent functional outcome compared with standard alteplase (79.5% vs 70.4%)—meeting criteria for both noninferiority and superiority—without significantly increasing the rate of symptomatic intracranial hemorrhage (ICH), researchers led by Shuya Li, MD, and Hong-Qiu Gu, PhD (both from Beijing Tiantan Hospital, Capital Medical University, China), report.
Although there were significantly greater risks of any intracranial hemorrhage, overall adverse events, and clinically relevant nonmassive hemorrhage in the reteplase arm, there were no differences in other bleeding outcomes or death.
The findings were published online recently in the New England Journal of Medicine to coincide with a presentation at the 10th Annual Conference of the Chinese Stroke Association & Tiantan International Stroke Conference 2024.
“The potential advantages inherent in reteplase lie in its favorable trade-off between efficacy and the risk of fatal bleeding,” the authors write. They cite findings from acute MI trials, including GUSTO III and RAPID II, which showed similar efficacy and safety with either reteplase or alteplase, noting that data have been lacking in the setting of acute ischemic stroke.
In addition to showing that reteplase was superior to alteplase in terms of functional outcomes, with similar safety, RAISE also demonstrated that reteplase increased the proportion of patients with early dramatic recovery of their NIHSS score.
“This finding suggests that the mechanism underlying the benefits of reteplase may involve a higher incidence of recanalization,” the investigators say.
The trial “raises the possibility of another intravenous thrombolytic drug that we could use to treat acute stroke patients,” Pooja Khatri, MD (University of Cincinnati, OH), commented to TCTMD, noting that this is the first phase III trial to address the topic.
A clinical impact, however, is likely further down the road. “It opens some doors, but we need more data to know if this is going to have a role in our armamentarium as part of our standard of care in the long run,” Khatri said.
Expanding Options
Alteplase has long been the standard of care when it comes to IV thrombolysis for acute ischemic stroke, but alternatives are emerging. Tenecteplase is the best studied, with mounting evidence supporting its use in this setting. Although it has not yet been approved for use in acute stroke by the US Food and Drug Administration, many centers have started swapping out alteplase for off-label tenecteplase primarily due to the ability to administer tenecteplase as a single bolus rather than as a 1-hour infusion.
But amid a growing demand for stroke thrombolysis, “the development of diverse, effective, and affordable thrombolytic agents is still needed,” Li, Gu, and colleagues say.
Like tenecteplase, reteplase has already been approved as a treatment for acute MI, but, in contrast, it has not been extensively studied for stroke thrombolysis. In a prior phase II trial by the Chinese investigators, reteplase—delivered as two boluses separated by 30 minutes—provided better functional outcomes without increasing fatal bleeding compared with alteplase.
To build on those findings, the investigators designed the phase III RAISE trial, which was conducted across 62 sites in China. They enrolled 1,412 patients ages 18 to 80 (median age 63 years; 70.5% men) who had a disabling ischemic stroke, could be treated within 4.5 hours of when they were last known to be well, were not slated to be treated with endovascular thrombectomy. Patients randomized to reteplase received two 18-mg boluses separated by 30 minutes and those randomized to alteplase received a standard infusion of 0.9 mg/kg over 1 hour (maximum dose 90 mg), with 10% of the dose delivered as an initial bolus.
It opens some doors, but we need more data to know if this is going to have a role in our armamentarium. Pooja Khatri
Overall the median NIHSS score at baseline was 6. A small number of patients—20 in the reteplase group and 25 in the alteplase group—received rescue thrombectomy. The median time from stroke onset to IV thrombolysis was 3 hours.
The primary efficacy endpoint was excellent functional outcome, defined as a score of 0 or 1 on the modified Rankin Scale (mRS), at 90 days. Reteplase increased the likelihood of reaching this goal compared with alteplase (risk ratio 1.13; 95% CI 1.05-1.21), a difference that met criteria for noninferiority due to the lower limit of the confidence interval coming in higher than 0.93 (P < 0.001); it also met the threshold for superiority (P = 0.002).
Also favoring reteplase were several secondary outcomes, including good functional outcome (mRS 0 to 2), the ordinal mRS shift, early dramatic recovery at 24 hours and 7 days, and a Barthel Index score of at least 95 at 90 days.
The primary safety outcome was symptomatic ICH within 36 hours of stroke onset. This was numerically, but not significantly, higher in the reteplase arm (2.4% vs 2.0%; risk ratio 1.21; 95% CI 0.54-2.75). The rate of any ICH at 90 days were greater with reteplase versus alteplase (7.7% vs 4.9%; risk ratio 1.59; 95% CI 1.00-2.51).
Reteplase also came with higher rates of any adverse events (91.6% vs 82.4%; risk ratio 1.11; 95% CI 1.03-1.20) and clinically relevant nonmassive hemorrhage (5.4% vs 2.4%; risk ratio 2.23; 95% CI 1.03-4.84), but there was no significant difference in 90-day mortality (4.3% vs 3.4%; risk ratio 1.25; 95% CI 0.66-2.35).
Possible Benefits of More Competition
Khatri pointed out that there are certain features to consider when interpreting the findings. In particular, she said, the age of participants was capped at 80 years, only about 30% of the cohort was female, and the overall severity of stroke appeared to be milder than in other trials. Moreover, there are higher rates of hemorrhagic stroke and intracranial disease in Chinese versus non-Chinese populations and there are likely differences in which patients are offered thrombectomy between China and other parts of the world.
“The background of care is not the same in China as here, so that’s another variable in all of this for generalizability,” Khatri said.
As for the outlook for use of reteplase in acute stroke, she said that there has been less enthusiasm for the agent than for Tenecteplase, because it is less fibrin-specific and is not as easy to administer.
Still, economic considerations may provide an opening for reteplase, Khatri speculated, noting that both alteplase and tenecteplase—the two main options for acute stroke—are made by the same company (Genentech).
“Expanding the market would generally be a positive thing in many ways if we were able to show these data to be generalizable for a broader stroke population,” she said. “Having more than one company that makes these drugs might create a more competitive market.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Li S, Gu H-Q, Li H, et al. Reteplase versus alteplase for acute ischemic stroke. N Engl J Med. 2024;Epub ahead of print.
Disclosures
- RAISE was supported by China Resources Angde Biotech Pharma, the National Key Research and Development Program of China, the National Natural Science Foundation of China, the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences, and the Beijing Municipal Science and Technology Commission. China Resources Angde Biotech Pharma provided reteplase and alteplase free of charge.
- Li and Gu report no relevant conflicts of interest.



Comments