Scaffold Thrombosis Concerns With Absorb BVS Echoed in AIDA Trial
Rates of definite stent thrombosis were fivefold higher with the newer technology, but some experts are still hoping to see benefits long-term.
Two-year results from the Amsterdam Investigator-Initiated Absorb Strategy All-Comers Trial (AIDA) show that use of the Absorb GT1 bioresorbable vascular scaffold (BVS, Abbott Vascular) is associated with a significantly increased risk of scaffold thrombosis, and of target-vessel MI, compared with patients who received an everolimus-eluting metallic stent (Xience, Abbott Vascular).
Unlike the 2-year results from ABSORB III, which were presented just 10 days ago at the American College of Cardiology 2017 Scientific Session, there was no significant difference in the risk of target-vessel or target-lesion failure among patients treated with the Absorb and Xience stents.
In total, definite/probable scaffold thrombosis occurred in 31 patients (3.5%) who received the Absorb device while stent thrombosis was documented in 8 patients (0.9%) who received the Xience stent (hazard ratio 3.87; 95% CI 1.78-8.42). The higher risk of scaffold thrombosis was evident in the subacute phase (>24 hours to 30 days) as well as late and very late phases, including beyond 1 year.
“It’s definitely a safety concern,” lead investigator Joanna Wykrzykowska, MD (Academic Medical Center, Amsterdam, the Netherlands) told TCTMD. “Actually, when you focus only on definite thromboses, the risk is five times higher with Absorb. When we did a landmark analysis of stent thrombosis at 30 days, the risk of definite and probable scaffold thrombosis was ongoing in the Absorb arm.”
Robert Byrne, MD (Deutsches Herzzentrum, Munich, Germany), who was not involved in AIDA, said the results are consistent with numerous studies, including several meta-analyses, showing Absorb BVS is associated with an increased risk of scaffold thrombosis. “On one level, it’s consistent and a little disappointing,” Byrne told TCTMD.
Actually, when you focus only on definite thromboses, the risk is five times higher with Absorb. Joanna Wykrzykowska
Another physician not involved in the study, B. Hadley Wilson, MD (Sanger Heart & Vascular Institute/Carolinas Healthcare System, Charlotte, NC), also called the results “sobering.” For him, the results are yet another reminder that physicians need to be extremely conscientious when implanting Absorb, paying particular attention to adequately preparing the vessel, appropriately sizing the device to the artery, and routinely postdilating patients to embed the scaffold struts into the vessel wall.
“In general, though, we’re going to have to inform the patient of this slightly increased risk of scaffold thrombosis and let them know we would probably recommend they stay on dual antiplatelet therapy longer than the 1 year that is normally recommended, as long as they’re tolerating that well,” said Wilson.
The study is published March 29, 2017 in the New England Journal of Medicine.
DSMB Recommends Early Report of Data
The AIDA study includes 1,845 patients undergoing routine PCI at five high-volume centers in the Netherlands. Speaking with TCTMD, Wykrzykowska said the trial had very limited exclusion criteria, with approximately 50% of patients presenting with acute coronary syndrome. Of those patients, 25% underwent primary PCI for acute myocardial infarction. Overall, the mean SYNTAX score was 13.2 (median 11.0), which is similar to trials such as LEADERS and RESOLUTE.
“It’s a randomized trial with Absorb BVS that included CTO lesions, heavily calcified lesions requiring rotoablation, and even some bypass grafts,” said Wykrzykowska. “It’s a pretty complex patient population.”
After the publication of disappointing 3-year results from ABSORB II, the AIDA investigators performed an interim analysis of their data in November 2016.
The only thing we do know and have evidence for is that the stent disappears. Robert Byrne
In ABSORB II, the 3-year data showed the Absorb BVS was associated with a two-fold increased risk of target-vessel myocardial infarction. That trial also showed an increased risk of scaffold thrombosis beyond 1 year with Absorb compared with Xience. Following the advice of the data safety and monitoring board (DSMB) to report the data early, AIDA investigators performed a “cross-sectional sweep of the data, collecting all the available events,” said Wykrzykowska. The current publication is an early report of the data owing to the safety concerns.
At 2 years, target-vessel failure, the study’s primary endpoint, occurred in 11.7% of patients treated with Absorb and 10.7% of patients treated with Xience, a difference that was not statistically significant. There was no difference in the risk of cardiac death between the two devices, but the risk of MI was significantly higher with Absorb BVS, including a higher risk of target-vessel MI (5.5% versus 3.2%; P=0.04). Target-vessel revascularization rates were not different between the two arms.
Regarding scaffold/stent thrombosis, 10 events occurred during the subacute phase with Absorb and two events were reported with Xience. From 31 days to 1 year, there were eight scaffold thromboses with Absorb and one stent thrombosis with Xience. During late follow-up (> 1 year to 2 years), there were nine additional scaffold thromboses compared with just two events in the Xience arm. One additional thrombotic event with Absorb occurred between 2 and 3 years.
To TCTMD, Byrne said these late events, which have been consistently observed in ABSORB II, ABSORB III, and ABSORB Japan, are the “surprise events,” the ones physicians and researchers weren’t expecting.
“This late safety signal is consistent so for us as physicians we have to ask ourselves what we do in patients receiving these stents and do we recommend a more prolonged duration of DAPT to ameliorate this risk,” said Byrne. “For those who have tolerated DAPT without any bleeding events, I think we have to leave them on it. For the ones who have already stopped DAPT, and who had tolerated it well, do we need to consider putting them back on it until the risk of these low-frequency but serious events seems to have ameliorated?”
Importance of Implantation Technique?
For Gregg Stone, MD (Columbia University Medical Center, New York, NY), who led the ABSORB III study, the results of AIDA are consistent with data from the ABSORB randomized trials. In an email to TCTMD, he noted that like these other trials, operators didn’t strictly adhere to the procedural techniques that are now known to be necessary to optimize BVS performance.
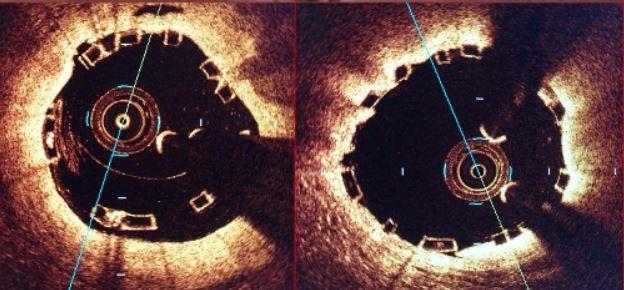
“Namely, post-dilatation at high pressure was not routine in AIDA, and avoiding treatment of small vessels was not emphasized,” said Stone. He also pointed out that intravascular ultrasound (IVUS) was used in only a small proportion of cases. “Numerous studies have now demonstrated that the -1 to 3-year results of BVS—the time frame of active bioresorption—can be optimized by enhanced technique,” he added.
Numerous studies have now demonstrated that the -1 to 3-year results of BVS—the time frame of active bioresorption—can be optimized by enhanced technique. Gregg Stone
Absent attention to diligent implantation techniques, Stone believes a 3-year duration of dual antiplatelet therapy is reasonable in patients not at a very high risk for bleeding.
Wykrzykowska said that in the trial, they prepared the vessel for implantation, which included predilatation with a noncompliant balloon, and appropriately sized the device to the vessel. At the time the study began, though, aggressive postdilatation of the implanted stent was not recommended by the instructions-for-use and as a result, 63% of patients were post-dilated in the first year of enrollment.
After the PSP strategy (Preparation, Sizing, and Postdilatation) was proposed as a way to reduce events, post-dilation was recommended to be performed routinely (from October 2014 onward) and the rate of postdilatation increased to 83% in the second year of enrollment.
“I must say, though, we have done some subanalyses and found that implantation technique does not really seem to influence the outcomes in AIDA, as was shown, for instance, in ABSORB III,” she said. “We still see clinical events in patients that underwent postdilatation.” The investigators also did not observe a difference in risk of thrombosis with vessels 2.25 mm or smaller compared with those with larger vessels.
What Now?
Wykrzykowska told TCTMD she agrees with the recent Food and Drug Administration (FDA) decision to send a safety alert to physicians—she believes they do need to be a little more cautious when using Absorb.
“I certainly don’t think that it’s a workhorse stent in clinical practice,” she said. “There are concerns about the risks of scaffold thrombosis and these have now been seen in several trials. So, if anybody uses it, it should be, perhaps, in fairly simple lesions with very careful lesion preparation and [optical coherence tomography] guidance to reduce the risks as much as possible. You also have to make sure that your patient can take long-term dual antiplatelet therapy.”
I certainly don’t think that it’s a workhorse stent in clinical practice. Joanna Wykrzykowska
Most importantly, she reminds physicians to “keep in the back of their mind” the important question of the long-term benefits of a dissolving stent. “Have we proven the putative benefits of BVS over metallic devices?” she questioned. “I think it’s a beautiful theory, but the 3-year follow-up of ABSORB II has raised a little bit of a question mark about this theory.”
Byrne agreed. “The only thing we do know and have evidence for is that the stent disappears,” he said, noting the theoretical advantages of Absorb weren’t observed at the 3-year mark in ABSORB II. “Improved vasomotion and late luminal expansion didn’t materialize, less angina didn’t materialize. . . . For me, there really isn’t a clear situation where you would say you’d prefer this scaffold over and above conventional, high-performance DES.”
In an editorial, Debabrata Mukherjee, MD (Texas Tech University Health Sciences Center, El Paso), also came to the same conclusion: “Given the lack of an advantage with respect to clinical efficacy, the challenges in delivering the device (including longer procedural times), and the higher rate of device thrombosis with the bioresorbable scaffold, there is little justification for routine use of the everolimus-eluting bioresorbable scaffold over the everolimus-eluting metallic stent.”
If it is used, Mukherjee said that 3 years of DAPT is needed, but this extended duration is likely to come at the higher cost of bleeding, which will further attenuate the potential longer-term benefits of Absorb BVS. The bottom line is that given how good the current-generation DES devices are, “there is little rationale to use bioresorbable scaffolds at this time.”
Byrne and Wykrzykowska stressed the technology is still in the early development phase and future iterations will emerge, which will hopefully address the device’s current issues. “The first step is identifying those problems so that we can learn from them and go further,” said Wykrzykowska.
Hadley added that he hopes the community does not interpret the results to suggest bioresorbable scaffolds are not a good way to go in the future. More refinements to device are needed, specifically thinner struts, but he remains optimistic about the technology.
Photo Credit: David Rizik, PSP: A Synthesis of Technique Imperatives for Absorb Implantation, TCT 2016.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Wykrzykowska JJ, Kraak RP, Hofma SH, et al. Bioresorbable scaffolds versus metallic stents in routine PCI. N Engl J Med 2017;Epub ahead of print. Mukherjee D. Device thrombosis with bioresorbable scaffolds. N Engl J Med 2017;epub ahead of print.
Disclosures
- Wykrzykowska reports receiving a grant from Abbott Vascular during the conduct of the study and personal fees from Abbott Vascular outside the submitted work.
- Stone reports consulting for Reva.
- Wilson reports no financial conflicts but served as the principal investigator at his site for ABSORB III and IV.
- Byrne and Mukherjee report no conflicts of interest.


Alexander Kharlamov