SCAI Updates Statement on Intracoronary Diagnostic Tools
The focused update to a 2014 consensus statement reflects the emergence of iFR and brings in new data on FFR, IVUS, and OCT.
(UPDATED) Incorporating evidence that has been accumulating over the past 4 years, the Society for Cardiovascular Angiography and Interventions (SCAI) has released a focused update to its 2014 consensus statement on the use of invasive assessments of coronary physiology and structure.
Authors led by Amir Lotfi, MD (Baystate Medical Center, Springfield, MA), introduced instantaneous wave-free ratio (iFR) to the document—and revised material dealing with fractional flow reserve (FFR), intravascular ultrasound, and optical coherence tomography (OCT).
Speaking with TCTMD, senior author Lloyd Klein, MD (Advocate Illinois Masonic Medical Center, Chicago, IL), said there hasn’t really been a change to the conclusions of the 2014 statement, which states that “these modalities are not indicated when noninvasive imaging and angiographic data are concordant or when the result of the additional procedure will not alter the planned treatment strategy or optimization of stent implantation.”
But the focused update, published online recently in Catheterization and Cardiovascular Interventions, was warranted because new data on iFR and additional findings on use of the other modalities in specific clinical scenarios have come out in recent years, he said.
A smaller society like SCAI is equipped to rapidly incorporate new information into recommendations, Klein said, noting that full practice guidelines take years to change.
“The interventional guidelines are outdated and don’t go into much of this at all. And even the appropriate use criteria, although they do mention FFR as something which should be used more often, [don’t] really talk about specific situations,” Klein said.
“Position statements and focused updates like this one,” he added, “can be really, really valuable in reflecting practice and leading the way toward further progress, more than guidelines or appropriate use criteria can.”
iFR and FFR
For iFR, DEFINE-FLAIR and iFR-SWEDEHEART showed that the technique is noninferior to FFR for guiding decisions about intervening on intermediate lesions in patients with stable angina or NSTE ACS.
Those data were good enough to convince the SCAI writers to include iFR in several recommendations alongside FFR. In patients with stable ischemic heart disease, for example, both iFR and FFR are deemed “definitely beneficial” for assessing the functional significance of intermediate coronary stenoses when noninvasive stress imaging isn’t available or doesn’t provide a definitive answer.
Another recommendation sees probable benefits when FFR or iFR are used to reclassify the number of vessels that are diseased in patients with multivessel disease, guiding the decision about whether to revascularize with CABG or PCI.
The authors also spend some time covering the utility of iFR and/or FFR in various situations, including stable ischemic heart disease, multivessel CAD, left main coronary stenosis, ACS, STEMI, aortic stenosis, tandem and serial lesions, and bypass grafts. They also discuss comparisons of iFR and FFR. “Obviously iFR is not as mature as FFR for evaluating intermediate lesions, but it’s pretty good, and I think that this really lays out the evidence for why iFR is a valuable tool,” Klein said.
Although much new material has been added regarding iFR, evidence has evolved for FFR over the last few years as well, and that’s reflected in the focused update. In particular, DANAMI3-PRIMULTI and Compare-Acute demonstrated that FFR-guided complete revascularization is beneficial in patients with STEMI.
Based on those findings, the authors say in the update that FFR may be valuable in determining which nonculprit lesions should be treated early and which can be safely deferred. “To the extent to which we’re going to be going toward performing nonculprit stenting in the acute setting either at the time of initial presentation or within 48 hours, I think that it’s almost impossible to see how that can be done without FFR and iFR,” Klein said, noting that “this is the first formal recommendation that I know of for FFR in the nonculprit lesion.”
IVUS and OCT
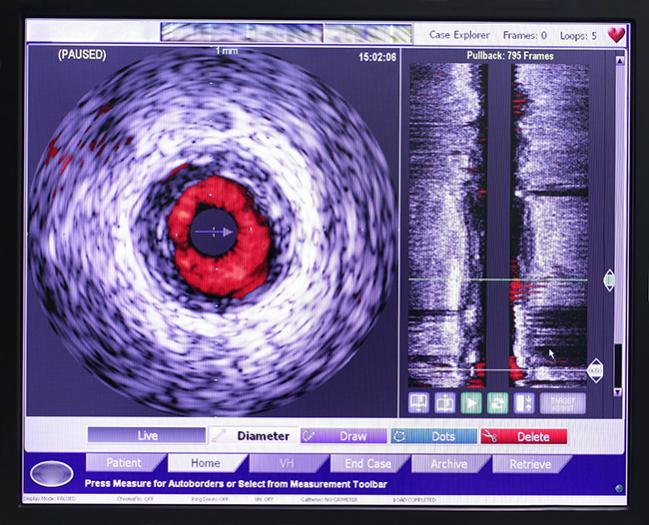
Also undergoing revisions were the sections on intravascular imaging with IVUS or OCT, both of which “offer excellent visualization of intraluminal coronary structure, particularly at the mural surface and lumen interface,” the authors say. “They may be especially useful in planning PCI strategy in high-risk subsets, such as left main stenosis, calcified lesions, and bifurcations.”
There are new “possibly beneficial” recommendations pointing out that meta-analysis have shown that using IVUS to guide PCI decreases major adverse events and, in long lesions, is associated with reduced MACE.
In addition, possible benefits for OCT now include assessments of the presence and extent of coronary dissection during PCI and of hazy lesions of uncertain etiology or severity or post-PCI suspected edge dissections.
“We still think that IVUS has value for determining stent expansion and for the left main lesion of indeterminate significance, and I think we need to say that [for] OCT in the interim of the last 4 years, there are studies that show that it’s really quite valuable qualitatively for evaluating edge dissection and plaque morphology,” Klein said.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Lotfi A, Davies JE, Fearon WF, et al. Focused update of expert consensus statement: use of invasive assessments of coronary physiology and structure: a position statement of the Society of Cardiac Angiography and Interventions. Catheter Cardiovasc Interv. 2018;Epub ahead of print.
Disclosures
- The authors did not report any information on potential conflicts of interest.


Comments