Signal of Impaired Sapien XT Durability in Midterm Follow-up
Sapien 3, on the other hand, is holding up just at well as surgical bioprostheses in midterm follow-up from PARTNER 2A.
Structural valve deterioration was documented in 8.8% of patients treated with Sapien XT at 5 years compared with just 3.5% of patients treated with surgery (P = 0.002).
In contrast, the rate of structural valve deterioration was not significantly different between the newer Sapien 3 device and surgical valve replacement. At 4 years, the longest follow-up available on the next-generation valve, the rate of valve deterioration was 2.6% in patients with the Sapien 3 valve compared with 2.5% among the surgical patients (P = 0.86).
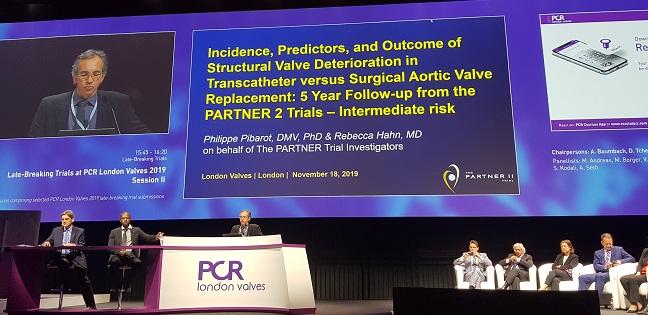
Philippe Pibarot, DVM, PhD (Quebec Heart and Lung Institute, Quebec City, Canada), who presented their analysis during the late-breaking clinical trial session at PCR London Valves 2019, said the results show that the second-generation Sapien XT is less durable than surgery whereas the newest valve is at least equivalent in midterm follow-up.
“Durability is the last Achilles’ heel, or the last unknown, for TAVR,” Pibarot told TCTMD. “We just got the results from the two latest trials in low-risk patients, which are encouraging, but on the other hand you think, ‘OK, but this is only 1 year.’ When we’re dealing with low-risk patients, you need to think 10 years from now. So, based on these results, we may need to careful with low-risk patients who are younger. When you’re younger than 65 years, maybe do surgery? SAVR is still a great operation when it’s well done and there is an established record for durability.”
PARTNER 2A and Sapien 3 Intermediate-Risk Registry
The new analysis included 2,032 intermediate-risk patients randomized to treatment with Sapien XT and surgery in the PARTNER 2A trial and 1,078 intermediate-risk patients treated with Sapien 3 as part of the S3 registry. The surgical arm from the PARTNER 2A trial served as the comparator for durability for the registry patients treated with Sapien 3.
Pibarot and colleagues assessed the rate of bioprosthetic valve failure using the standardized definition from the European Association for Cardio-Thoracic Surgery/European Association of Percutaneous Coronary Intervention (EACTS/EAPCI). The definition of structural valve deterioration, which includes the presence of abnormal valve leaflet morphology and mobility, was modified slightly to require a documented increase in the mean pressure gradient in echocardiographic follow-up (as opposed to using a single measure of increased mean pressure gradient). To TCTMD, Pibarot said they modified the definition to exclude patients with severe prosthesis mismatch who may have a high gradient but completely normal valve function.
Overall, the rate of bioprosthetic valve failure was 3.7% with Sapien XT at 5 years versus 0.5% with surgery (P = 0.002). In contrast, the rate of valve failure at 4 years was 0.6% with Sapien 3, which was not significantly higher than that observed with surgery at the same time point (P = 0.58). The combined endpoint of structural valve deterioration or bioprosthetic valve failure was 9.5% with Sapien XT at 5 years and 3.5% with surgery (P < 0.001). In contrast, the combined rate for Sapien 3-treated patients was 2.7% at 4 years (P = 0.74 versus surgery).
For Philippe Généreux, MD (Morristown Medical Center, New Jersey), these new data should sooth any fears about valve durability, rather than heighten them, particularly since Sapien 3 is a contemporary valve used in current clinical practice.
“Sapien 3 is the valve we use today, and it’s the one that has the best performance in terms of paravalvular leak,” he said. “You can also argue that the Sapien 3 Ultra, which has a little more ‘skirt,’ will show even better results. I think these results show us similar durability between Sapien 3 and surgery, but the real data set that will give us the final answer is PARTNER 3. These are lower-risk patients, maybe a little more active. I think we’ll learn more in the future, but these data for me are very reassuring.”
In the meantime, said Généreux, the PARTNER 2A data show the device is a solid transcatheter heart valve and patients should be comforted by these midterm results, he said.
To TCTMD, Janarthanan Sathananthan, MBChB (St. Paul’s Hospital, Vancouver, Canada), said valve durability is a hot-button issue raised at nearly every interventional cardiology meeting, but that the only way operators will know if a device is truly durable is to study patients for long periods of time, which in itself is a problem.
“I don’t know if we’re going to actually resolve the durability issue with transcatheter valves any time soon,” he said. “One reason, in my mind, is that the technology is just moving so rapidly. If you take current contemporary devices, Sapien 3 or Evolut R [Medtronic], and say we need to wait 10 years in low-risk patients to determine if the valves are fine, in 10 years we’re going be on to our sixth-, or seventh-, or eighth-generation platforms. We’re going to be saying we don’t use those valves anymore.”
Why the Difference Between Valves?
Michael Borger, MD, PhD (Leipzig Heart Center, Germany), a cardiovascular surgeon who participated in the panel discussion following the PARTNER 2A presentation, also considers the results encouraging in that durability with Sapien 3 looks good thus far. Still, he questioned how device modifications from the second-generation device to Sapien 3 could have had such an impact.
“The changes made from the Sapien XT to Sapien 3 were a basically smaller sheath and the addition of the cuff,” he said. “It’s expected you’d have less paravalvular leak, but I don’t understand why the structural valve deterioration rates are better. If the pressure gradients, if the amount of turbulent flow across the valve is similar, which we know from previous studies . . . then the [structural valve deterioration rates] should be similar.”
Pibarot suggested there are differences in design, including changes that contribute to better valve deployment, expansion, and positioning with the current-generation device. Additionally, CT was not used routinely to size the valve in PARTNER 2A whereas it is used consistently in patients treated with Sapien 3. Given concerns about paravalvular leak with Sapien XT, operators were also more likely to “oversize” the valve by placing a larger device in a smaller annulus.
“All the changes in design and the sizing strategy between Sapien XT and Sapien 3 contributed to some extent to reduce the mechanical stress on the leaflets,” said Pibarot. “All these factors contribute to better durability.”
Michael Mack, MD (Baylor Scott & White Health System, Plano, TX), one of the PARTNER 2A investigators, also emphasized the lack of routine CT imaging in PARTNER 2A and increased paravalvular leak as possible contributing factors to the worse durability with Sapien XT. “There is some thought that paravalvular leak leads to structural valve deterioration,” he told TCTMD. “Also, there is less postdilatation [with Sapien 3] after deployment. There is still some concern that if you dilate with a balloon afterwards, you damage the leaflets. Do that less, and you damage the leaflets less.”
Regardless of the reason, Mack believes the impaired durability with Sapien XT is real. The 5-year data from PARTNER 2A did show an advantage with surgery over TAVR, he noted, and durability might explain why the TAVR-treated patients didn’t do as well. As reported previously, the rate of death or disabling stroke at 5 years was 47.9% in patients treated with the Sapien XT and 43.4% in those who underwent surgery (P = 0.21).
From a clinical perspective, Mack and Pibarot both recommend annual follow-up for patients implanted with Sapien XT.
In patients with an increased pressure gradient, Pibarot said they should be followed a little more closely, possibly every 6 months. “When there is some valve dysfunction, it can accelerate, and you don’t want to miss the sweet spot to intervene,” he said. Mack added that patients who have received an XT device are further along in follow-up so extra vigilance is warranted. “You worry about them more at 6, 7, or 8 years than you did at 2 or 3 years,” said Mack.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Pibarot P, on behalf of the PARTNER 2 investigators. Incidence, predictors, and outcomes of structural valve deterioration in transcatheter versus surgical aortic valve deterioration: 5-year follow-up from the PARTNER 2 trials. Presented at: PCR London Valves 2019. November 18, 2019. London, England.
Disclosures
- Pibarot reports research support and/or consulting fees from Edwards Lifesciences, Medtronic, Cardiac Phoenix, V-Wave, and Edwards Lifesciences.
- Généreux reports consulting for, receiving speaking fees from, or holding equity in Abbott Vascular, Abiomed, Boston Scientific, Cardinal Health, Cardiovascular Systems Inc., Edwards Lifesciences, Medtronic, Opsens, Pi-Cardia, Puzzle Medical, Soundbite Medical, SIG.NUM, Saranas, Siemens, and Tryton Medical.
- Sathananthan reports consulting fees/honoraria from Edwards Lifesciences
- Mack served as the coprincipal investigator of the PARTNER 3 trial and COAPT trials. He reports consulting for Gore.


Comments