‘Super-Dense’ Calcified Plaque Appears Protective Against ACS
Identifying these so-called 1K plaques could help fine-tune risk stratification in patients undergoing coronary calcium scoring.
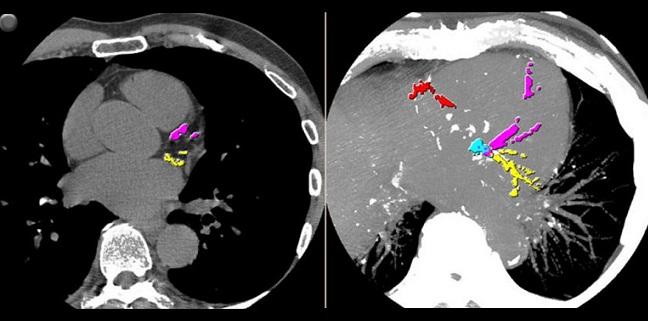
High-density plaque identified on coronary computed tomography angiography (CCTA) is associated with a lower risk of acute coronary syndrome, a finding that suggests increasing density is indicative of greater plaque stability, say researchers.
In a case-control study, those who had an ACS had significantly less high-attenuation coronary plaques, which were dubbed 1K plaques because the measured Hounsfield units (HU) exceeded 1,000 units, a reflection of dense calcification, when compared with control subjects who did not have an event.
Led by Alexander van Rosendael, MD (Leiden University Medical Center, the Netherlands), and senior investigator Leslee Shaw, PhD (NewYork-Presbyterian Hospital/Weill Cornell Medical College, New York, NY), the new study, which was published online January 22, 2020, in JAMA Cardiology, suggests that differentiating the type of coronary plaque could help further identify patients at risk for clinical events.
“What we’ve started to understand in recent years, especially with coronary artery calcium [CAC] scoring, is that the more plaque there is, the worse prognosis,” van Rosendael told TCTMD. “If you have a lot of plaque, your risk is very high. Now we’re starting to ‘fine-tune’ this plaque a little bit more. It’s not just about plaque burden, but differences in plaque density.”
Van Rosendael noted that coronary plaque density has been previously shown to be associated with a lower risk of clinical events in the MESA study, a finding that was observed in multiple subgroups, including patients with diabetes. Histologic studies have also shown stable coronary lesions tend to be more densely calcified while unstable coronary plaques are characterized by fibroatheromas consisting of large necrotic cores, lipid-rich plaques, and inflamed fibrous caps.
On CT, these 1K plaques appear “super white and super dense,” said van Rosendael, and do not include any other type of material, such as noncalcified or soft plaques. “These 1K plaques are super calcified and that’s it,” he said.
More Densely Calcified, Greater Plaque Stability
To study the association between plaque density and clinical risk, the researchers analyzed data from the Incident Coronary Syndromes Identified by Computed Tomography (ICONIC) study, which was a nested case-control study made up of patients with no known coronary artery disease included in the Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter (CONFIRM) registry. In CONFIRM, patients who underwent CCTA for suspected coronary artery disease were monitored for the occurrence of major adverse cardiovascular events. The study population included 189 patients who had an ACS and 189 propensity score-matched control subjects (mean age 59.9 years; 65.3% male).
These 1K plaques are super calcified and that’s it. Alexander van Rosendael
The total mean calcified plaque volume was not significantly different between ACS patients and control subjects. The mean volume of 1K plaque was 3.9 mm3 in ACS patients and 9.4 mm3 in controls (P = 0.02). In an analysis restricted to patients who had an MI, these patients also had a mean volume of 1K plaque that was significantly less than the control group (3.6 vs 10.0 mm3; P = 0.01). Individuals with the most 1K plaque, by quartile, had more calcified plaque and less necrotic core/fibrofatty plaque than those with less-dense calcification.
The researchers also performed a lesion-level analysis in 93 subjects in whom a precursor lesion for future ACS could be identified on CCTA. The culprit precursor lesion in the ACS patients had a lower mean volume of 1K plaque than coronary lesions with greatest coronary stenosis in controls (2.6 vs 7.6 mm3; P = 0.01).
Khurram Nasir, MD (Houston Methodist DeBakey Heart & Vascular Center, TX), a proponent of CAC scoring who wasn’t involved in the ICONIC analysis, said pathophysiology studies have shown that as coronary plaque becomes more densely calcified, the more stable it becomes. At the same time, however, the overall plaque burden may increase. This is the CAC paradox, said Nasir, in that there are improved clinical outcomes in patients with coronary plaque progression as long as that progression is marked by increasingly dense calcification.
“There is definitely room for reducing the heterogeneity of risk by looking at the plaque density, as MESA has also shown recently,” he said. “For example, if you have a calcium score greater than 400, about 20% to 30% will have an event in the next 30 years, but the majority won’t. It’s quite likely that in looking at individuals with these high calcium scores who don’t have an event it’s because a lot of their plaque would be more densely calcified or stabilized plaque.”
Nasir stressed, however, that an increasing CAC score does not equate to a larger percentage of densely calcified lesions. In a 2010 study, for example, he looked at the variation in atherosclerotic plaque composition according to increasing CAC scores and showed that patients with a higher CAC score were more likely to have coronary plaques made up of a combination of calcified, noncalcified, and mixed plaques. These mixed plaques are strongly associated with myocardial ischemia and adverse clinical outcomes, said Nasir.
“The higher the calcium score—whether going from 0 to 10, or 10 to 100, or 100 to 1,000—there really is no point where the risk levels off,” said Nasir. “One would expect the higher calcium score, the more stable plaque you would have, and then you would have a lower risk of events. We never see that. . . . If you have a higher calcium score, you’re more likely to have a lot of unstable plaques with a mixed composition.”
Clinical Utility of Plaque Density
To TCTMD, van Rosendael said they are currently studying the effect of statin therapy on plaque density in roughly 2,000 patients included in the Progression of Atherosclerotic Plaque Determined by Computed Tomographic Angiography (PARADIGM) study. Their preliminary results suggest that statins increase 1K plaque, but not low-density calcification. “It supports the idea that this 1K is a protective plaque,” said van Rosendael.
In an editorial, Michael Criqui, MD, Isac Thomas, MD (both University of California, San Diego), and Nketi Forbang, MD (US Department of Defense/Veterans Affairs Extremity Trauma and Amputation Center of Excellence Naval Health Research Center, San Diego), point out that CAC has been shown to be “the strongest single marker of coronary artery disease risk,” and that combining CAC volume and density accounts for more risk than when combining all the risk factors that make up the standard atherosclerotic CVD risk equation (total and HDL cholesterol, systolic blood pressure, hypertension medication use, diabetes, and current smoking).
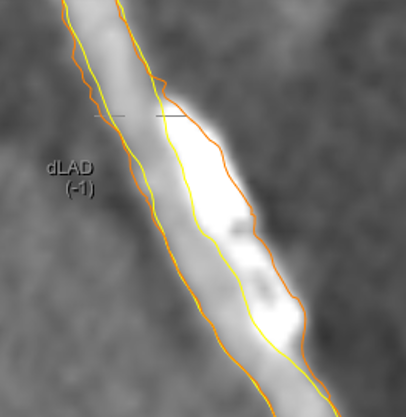
yellow = lumen. Orange = vessel wall.
Photo Credit: Alexander van Rosendael.
“The ICONIC authors concluded that measurement of 1K plaque may improve risk stratification beyond plaque burden,” write the editorialists. “We agree but wonder whether it will have any therapeutic implication. Patients with known CAD should receive maximal preventive therapy in any case. However, new attention to the associations of plaque density may be useful.” For example, evidence suggests that statins increase calcification and reduce the necrotic core, which in turn stabilizes the plaque.
Measuring plaque density is a painstaking, time-consuming process, said Nasir, which makes the clinical application of these findings a challenge at the present time. However, if the characterization of plaque density could be automated, then it would offer some clinical utility. “For example, if I have two patients with very high calcium scores, but one has mostly dense, heavily calcified plaques, it would allow me to be slightly more flexible in treating those with more-stable calcified plaques and more aggressive in those with less-dense plaques.”
Photo Credit: Radiological Society of North America
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Van Rosendael AR, Narula J, Lin FY, et al. Association of high-density calcified 1K plaque with risk of acute coronary syndrome._ JAMA Cardiol_. 2020;Epub ahead of print.
Criqui MH, Forbang NI, Thomas IC. The importance of coronary artery calcium density. JAMA Cardiol. 2020;Epub ahead of print.
Disclosures
- Van Rosendael, Criqui, Forbang, Thomas, and Nasir report no relevant conflicts of interest.


Arreka Jorkman
Arreka Jorkman