Tailored TAVI: Standardizing Balloon Pressures May Curb Operator Angst
The technique is a good start, but it needs to be tested in larger and more diverse patient populations, one expert suggests.
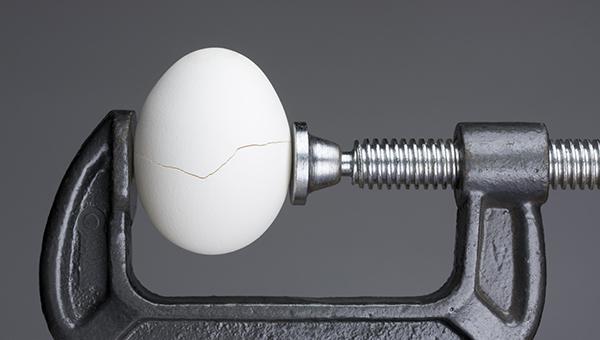
A pressure-regulated method for deploying balloon-expandable aortic valves can minimize the risk of annular injury without compromising TAVI technique or success, even in patients at high risk for rupture, according to results of an Australian study.
“Our method of pressure-regulated deployment of balloon-expandable transcatheter heart valves significantly improves and simplifies current protocols by ensuring that each valve prosthesis is deployed at the optimal pressure to enable optimal apposition between the valve and the aortic annulus, thereby minimizing [paravalvular regurgitation (PVR)] while also minimizing risk of aortic injury,” Ng noted. “Importantly, our innovation dramatically simplifies and takes the anxiety out of the process of getting the optimal outcome in balloon-expandable TAVR.”
As part of the study, Ng and colleagues led by Afik Snir, MBBS (University of Sydney, Australia), defined targets for stress exerted on the annular wall during deployment of 23 mm, 26 mm, and 29 mm balloon-expandable valves. No cases of rupture were seen with the pressure-regulated strategy when wall stress stayed within the targets.
The postdilatation rate was low at 10%, and mild PVR occurred in 12.7%, with no severe PVR. To TCTMD, Ng said the ability of the technique to keep PVR low is increasingly relevant as TAVI becomes available for lower-risk and younger patients.
The study was published online October 26, 2021, ahead of print in JACC: Cardiovascular Interventions.
Improving Optimization of TAVI
For the study, Snir and colleagues included 330 patients who underwent TAVI with Sapien 3 devices (Edwards Lifesciences) between August 2015 and July 2020. Of those, 106 patients were considered at high risk of annular rupture. All had preprocedural computed tomography and transthoracic echocardiography (TTE).
The optimal safety range of deployment wall stress was defined as 3-3.5 MPa. Compared with a wall stress of ≤ 3 MPa, patients with valves deployed at a wall stress > 3 MPa had lower rates of postdilatation (9.4% vs 32.0%; P < 0.001) and lower rates of PVR on TTE (11.4% vs 22.7%; P = 0.014). In the entire cohort, PVR was none/trivial in 81.2%, mild in 17.1%, and moderate in 1.7%.
No association was seen between wall stress and rates of new permanent pacemaker insertion or new persisting left bundle branch block.
Two cases of annular rupture occurred during the study. Both included subannular calcification with wall stress during the procedure of 3.69 MPa and 3.84 MPa, respectively.
Commenting on the results for TCTMD, Marwan Saad, MD, PhD (Brown University, Providence, RI), said the pressure-regulated technique is a valuable addition to the TAVI literature that, with further study, may turn out to be a particularly good option for those at high risk of annular rupture.
“These are patients with a lot of calcification of the annulus and the leaflets where you're fighting between reaching an optimal size that prevents paravalvular regurgitation, but also prevents annular rupture,” he said. “We need to see this technique used in other, larger patient populations, but it looks to be something that is very predictable and reproducible.”
Practical Implications for Use
In an accompanying editorial, however, John Webb MD, and Janarthanan Sathananthan, MBChB, MPH (both St Paul’s Hospital, Vancouver, Canada), argue that a pressure-regulated strategy has limited usefulness given the low percentage of patients at risk for annular rupture.
“So, it seems that for a relatively small number of patients with CT assessable adverse root features such as subannular calcium, protuberant nodules, bicuspid or bulky calcified leaflets, small annuli, or very advanced age a pressure-regulated expansion strategy might have something to offer,” Webb and Sathananthan observe. In the absence of subannular calcium, they add, the risk of rupture is remote.
Webb and Sathanathan give the example of a patient with an annular size at the border zone of two valve sizes, noting the operator dilemma of either choosing a smaller valve and accepting greater PVR, or choosing a larger valve and accepting greater risk of annular rupture.
Ng, however, pushed back. “We respectfully but strongly disagree with Drs. Webb and Sathananthan. I strongly stress that our technique is highly applicable to all TAVIs, as it simplifies the deployment protocol and results in more consistent, safe and effective outcomes,” he said.
“Our study shows that the pressure-regulated technique simplifies TAVR sizing choice and deployment strategy in this common scenario,” Ng observed. “For example, if one chooses the larger valve in a border zone case, deployment of the [transcatheter heart valve] at the optimal pressure will ensure optimal expansion without significant risk of annular rupture. Once again, the safety and efficacy of the pressure-regulated method simplifies the clinical decision-making and enhances the TAVR outcome in this common clinical scenario.”
I don't think anybody had thought about this before, and I think it's going to definitely provoke a lot of discussions. Marwan Saad
Saad said he also thinks the technique may be widely applicable beyond just those at high risk of rupture. One population he would like to see the strategy tested in, but not included in the current study, are patients with a previous surgical valve replacement undergoing valve in-valve TAVI.
“This cohort is pretty important because in a lot of cases, we try to fracture the surgical frame of the older valve to achieve the least gradient,” Saad noted. “In doing so, we put a lot of volume and increased pressures inside the TAVR valves to try to fracture these old surgical frames, and that definitely has high risk of annular rupture, even more than native valves.”
Overall, Saad said he sees the proposed technique as a fresh way of approaching TAVI optimization.
“I don't think anybody had thought about this before, and I think it's going to definitely provoke a lot of discussions,” he said. “But, before reaching conclusions and adopting this technique on a daily basis, we have to use it in a larger number of patients and confirm it in randomized trials.”
Webb and Sathananthan argue that more intermediate valve sizes would help operators make better sizing decisions, noting that the balloon-expandable Myval (Meril Life Sciences), for example, is available in many countries with diameters ranging from 20 mm to 29 mm in smaller 1.5-mm increments.
However, Saad noted that from an industry standpoint, offering a range of sizes that are not going to be widely used may not be attractive financially. Even with more sizes available, said Ng, the study findings that optimal expansion of a balloon-expandable valve is fundamentally determined by biomechanical forces (ie, wall tension) between the valve and the patient’s annulus holds true.
“If there are indeed more valve sizes in the future, their optimal deployment will also be determined by achieving the ideal pressure,” he concluded.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Snira A, Wilson MK, Ju LA, et al. Novel pressure-regulated deployment strategy for improving the safety and efficacy of balloon-expandable transcatheter aortic valves. J Am Coll Cardiol Intv. 2021;Epub ahead of print.
Webb J, Sathananthan J. Is it time for bespoke TAVR? J Am Coll Cardiol Intv. 2021;Epub ahead of print.
Disclosures
- Snir and Saad report no relevant conflicts of interest.
- Ng reports a research grant from Edwards Lifesciences for a project unrelated to the current study.
- Webb reports being a consultant to, and receiving research funding from, Edwards Lifesciences, Abbott, and Boston Scientific.
- Sathananthan reports being a consultant to Edwards Lifesciences and Medtronic and receiving speaking fees from Edwards Lifesciences and NVT.




Comments