Takotsubo Syndrome Not Necessarily ‘Benign’ or Fleeting
Certain patients should be followed closely for years since Takotsubo doesn’t always automatically revert to normal, a large meta-analysis suggests.
Long-term rates of mortality and recurrence following an index Takotsubo syndrome event are not negligible, and older age, physical stress, and atypical ballooning at presentation are each associated with worse prognosis, according to a new systematic review.
“In real-world clinical practice worldwide, the long-term outcome of Takotsubo syndrome is not so benign as previously thought,” lead author Francesco Pelliccia, MD, PhD (La Sapienza University, Rome, Italy), told TCTMD. “It's [not as bad] as those who suffer from acute myocardial infarction, but it's much worse than [the] mortality of the general population. So these patients should be followed closely for years after the acute phase.”
Published online last week ahead of print in JACC: Heart Failure, the analysis by Pelliccia and colleagues included 54 studies of 4,679 patients (87% women) around the world who were admitted to the hospital with Takotsubo syndrome between 2006 and 2017. Emotional and physical stressors were each noted in just over one-third of patients, and chest pain was reported in two-thirds.
Death during the index admission occurred in 2.4% of patients. Of those who were discharged, 10.2% died within a median follow-up of 28 months (22% because of cardiac issues), making the annual rate of total mortality 3.5%. The adjusted annual incidence of recurrence of Takotsubo syndrome was 1.0%.
On meta-regression analysis, long-term mortality was associated with older age (P = 0.05), physical stress (P = 0.001), and atypical ballooning at presentation (P = 0.009).
We have to pay attention to these patients, because it is not just an accident that if you survive the acute phase that you revert to normal. Francesco Pelliccia
These findings are mostly confirmatory of prior research, but Pelliccia said he was surprised to see that atypical ballooning led to worse prognosis. “It's not true anymore that Takotsubo syndrome always is associated with reversal to normal [for] the left ventricle,” he said. “There are now data showing that after an episode of Takotsubo syndrome, there are subtle but detectable changes in the left ventricular morphology and the function. So . . . when we say that the atypical ballooning forms were associated with the worse outcome, we mean that if the heart suffers from a greater extent of damage during the acute episode, probably it won't be able to repair to normal, as commonly believed.”
In an accompanying editorial, L. Christian Napp, MD (Hannover Medical School, Germany), commended the researchers for their “laborious effort” in conducting the study, noting its importance since “many reports on Takotsubo syndrome and its prognosis are based on single cases or small series and have limited follow-up. . . . As such, the study is complementary to outcome data from multicenter registries.”
In the past few years, “the picture of Takotsubo syndrome has undergone significant reshaping,” he writes. “The present study adds important knowledge about prognosis of patients with Takotsubo syndrome. Because the vast majority of studies on Takotsubo syndrome are more or less retrospective in nature, reported prognosis varies, even if we have matched data. We can conclude that Takotsubo syndrome carries considerable risk, especially if a physical trigger is present, and it is not a ‘self-healing syndrome.’”
We can conclude that Takotsubo syndrome carries considerable risk, especially if a physical trigger is present, and it is not a ‘self-healing syndrome.’ L. Christian Napp
Open questions persist, however. “What remains to be defined is the optimal therapy during follow-up in acute phase,” Pelliccia commented to TCTMD. “We actually do not have any definite data about this. . . . The next step will be to collect in a more accurate way than before data on the effect of medical therapy after an acute phase of Takotsubo syndrome.”
Also, “just a few studies have focused on what happens when these patients are discharged alive after the index event,” he added. “We have to pay attention to these patients because it is not just an accident that if you survive the acute phase that you revert to normal. No, this is not the truth. You are prone to experience repeat events of Takotsubo syndrome, and your prognosis is not that good.”
Napp agrees. “To answer the open questions, we should aim for prospective studies with comprehensive data acquisition in the acute phase and systematic follow-up including the cause of death,” he writes. “Given the existing recurrence rate and the still huge amount of beta-blockers prescribed without data, studies aiming to test medical therapies are needed.”
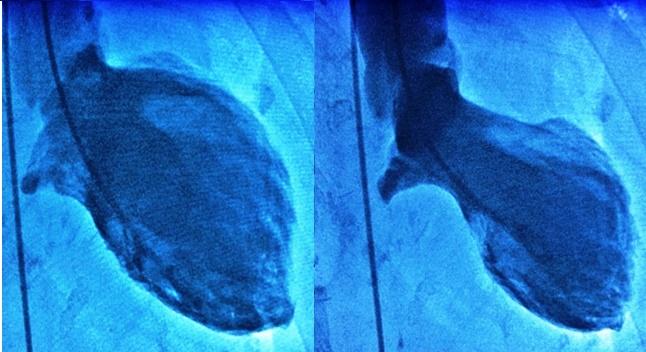
Photo Credit: Francesco Pelliccia. Pictured: Typical left ventricular end-diastolic (left panel) and end-systolic (right panel) angiographic images in a patient with Takotsubo syndrome.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Pelliccia F, Pasceri V, Patti G, et al. Long-term prognosis and outcome predictors in Takotsubo syndrome: a systematic review and meta-regression study. J Am Coll Cardiol HF. 2019;Epub ahead of print.
Napp LC. The risk of Takotsubo syndrome: seeing the light. J Am Coll Cardiol HF. 2019;Epub ahead of print.
Disclosures
- Pelliccia reports no relevant conflicts of interest.
- Napp reports receiving modest personal fees for lectures, proctorship, consulting or travel support from Abiomed, Maquet, Cytosorbents, Bayer, Zoll, Amgen, Biotronik, Merit Medical, Servier, and Terumo.


Comments