Three Years On, Absorb BVS Still Doesn’t Improve Myocardial Blood Flow
These new data throw cold water on the idea that a dissolved scaffold would lead to a healthier vessel and improved perfusion.
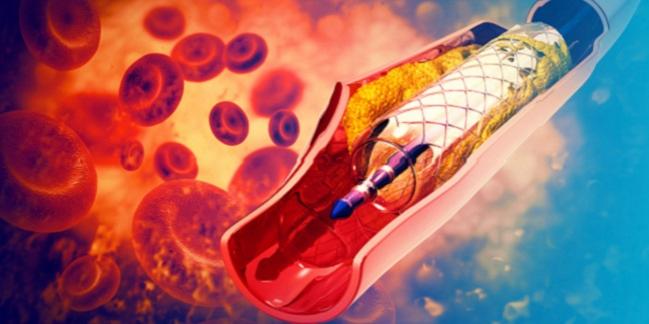
Three years after PCI, there is no significant difference in myocardial perfusion among patients who received the now-discontinued Absorb bioresorbable vascular scaffold (BVS; Abbott Vascular) compared with those who received a conventional drug-eluting stent, according to the results of the VANISH study.
The Absorb device should have been completely degraded at 3 years, which would allow the artery to heal and assume its normal geometry, but the present study challenges the hypothesized beneficial effects of scaffold resorption given the lack of improvement in myocardial blood flow, say investigators.
“The results are disappointing in the sense that the whole hypothesis—based on the idea that degradation of the scaffold would lead to a healthier vessel, which would translate into increased perfusion—was not the case in this study, which was meticulously done,” senior investigator Paul Knaapen, MD, PhD (VU University Medical Center, Amsterdam, the Netherlands), told TCTMD. “It’s not a very large study, but in terms of a randomized trial with positron emission tomography [PET]—three scans and two cath lab studies over 3 years—it is quite extraordinary and not likely to be reproduced soon. Nor does it need to be.”
The Absorb BVS story never delivered the hoped-for happy ending. The bioresorbable scaffold first received CE Mark approval in Europe in 2011, but a series of studies swiftly followed flagging an increased risk of thrombotic events, and the device was eventually restricted to European centers participating in clinical registries. In the United States, the scaffold was approved in 2016, but the Food and Drug Administration soon issued weighty warnings that highlighted the increased risk of major adverse cardiac events among patients who receive the scaffold.
In September 2017, Abbott Vascular halted commercial sales of the device and Absorb BVS was officially discontinued.
Tommaso Gori, MD, PhD (University Medical Center, Mainz, Germany), who was not involved in the current study, pointed out that this latest work dovetails with that of the ABSORB II study. In that analysis, investigators also assessed angiographic vasomotor reactivity and showed that endothelial function was not improved 3 years after treatment with the BVS. While next-generation resorbable scaffolds are in the works, Gori isn’t optimistic about the technology given these new findings showed no improvement in endothelial-dependent vasodilation.
“This study, along with ABSORB II, shows the concept of bioresorbable scaffolds is nice as a concept but for the moment there is no real evidence they provide a benefit,” he told TCTMD.
Patients Doing Fine, but No BVS Benefit
VANISH, which was published April 24, 2019, in JACC: Cardiovascular Interventions, included 60 patients aged 18 to 65 years with single-vessel disease and straightforward lesions (type A or B1) randomized to treatment with Absorb BVS or an everolimus-eluting metallic stent (Xience or Xience Prime; Abbott Vascular). In total, 59, 56, and 51 patients underwent cardiac PET imaging at 1 month, 1 year, and 3 years, respectively, to assess myocardial blood flow during rest, hyperemia, and cold pressor testing, which is performed to evaluate sympathetic function.
The primary endpoint of the study—the interaction between the device type and time—was not significant for hyperemic myocardial blood flow, endothelium-dependent vasodilation by cold pressor testing, and coronary flow reserve. In all patients, hyperemic myocardial blood flow decreased from 1 to 3 years, while coronary flow reserve was lower at 3 years compared with testing at 1-month and 1-year follow-up.
I see a theory, but no empirical data supporting the biological rationale. Tommaso Gori
“We had to have a stent that would biodegrade, that would do the job to recover coronary flow and then dissolve over time,” said Knaapen, referring to the promise of bioresorbable technology. “One of the potential beneficial effects was that we could get a return of vasomotor function. As the scaffold dissolved, you’d get back vasoconstriction and vasodilation of the coronary arteries, which would ultimately improve myocardial perfusion. That’s ultimately why we place stents—to improve perfusion to the myocardial muscle.”
As part of the trial, the researchers also performed optical coherence tomography (OCT) during the index procedure and at 3 years. Knaapen noted that OCT imaging revealed the scaffold still hadn’t completely degraded by 3 years, which might partly explain why they didn’t observe an improvement in myocardial blood flow. “We saw a breakdown but also a lot of residual stent fragments, which potentially interfered with the vasomotor function of the coronaries,” he said.
One downside of Absorb BVS has always been strut thickness, with Absorb significantly thicker than the latest-generation DES. On quantitative coronary angiography, the acute luminal gain after device implantation was lower with Absorb than with DES, which resulted in a lower minimal lumen diameter and increased percent diameter stenosis after PCI, although this difference was no longer observed at 3 years. The OCT analysis showed a significant decrease in the minimal lumen area from immediately after PCI to 3 years in the Absorb-treated patients, but not in the Xience arm.
Knaapen stressed there were no complications in the treated patients, which he attributes to their inclusion criteria that only allowed patients with simple lesions in large vessels to be randomized. “Our patients are doing fine,” he said. “It’s just that they appear, up until this point at 3 years, not to have any benefit of the scaffold as opposed to a metallic drug-eluting stent.”
‘Extinct Before It Had a Chance to Evolve’
In an editorial accompanying the new study, Grzegorz Kaluza, MD, and Juan Granada, MD (Cardiovascular Research Foundation, New York, NY), turn a critical eye towards the early enthusiasm for bioresorbable scaffolds, noting that European approval was based on relatively little data. Even though the larger trials, such as ABSORB II and III, were still enrolling patients, the scaffold was “optimistically incorporated into clinical practice despite the scarcity of clinical data,” they say.
To TCTMD, Gori pointed out that use of Absorb BVS in these settings, and even implanting the device without using the PSP protocol (lesion preparation, appropriate sizing, and postdilatation), emphasized the shortcomings of the first-generation scaffold. On the flip side, it also served to raise these issues early.
“Absorb evolved over time,” said Gori. “To me, what killed the technology was not ABSORB III or AIDA, but rather the evidence that you need extreme precautions at the time of implantation. You cannot bring a device which requires extra precaution to the general market, [because] there will always be physicians who do not respect the extended [conditions] for use.”
“Excessive clinical expectations based on overthought theoretical presumptions have made a potentially valuable technology nearly extinct before it had a chance to evolve,” they write. Nonetheless, they express some hope that bioresorbable scaffolds, while not a panacea for atherosclerosis, can become a reality if the technology can overcome some of the first-generation hurdles.
Going forward, Gori noted that next-generation devices won’t be approved without extensive testing, and this includes long-term safety and effectiveness data. The other hurdle is that VANISH, as well as ABSORB II, refute the biological underpinnings for resorbable scaffolds. “I see a theory, but no empirical data supporting the biological rationale,” he said.
Note: Kaluza is an employee of the Cardiovascular Research Foundation (CRF), the publisher of TCTMD, and Granada is CRF’s president and chief executive officer.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Stuijfzand WJ, Schumacher SP, Driessen RS, et al. Myocardial blood flow and coronary flow reserve during three years following bioresorbable vascular scaffold versus metallic drug-eluting stent: VANISH trial. J Am Coll Cardiol Intv. 2019;Epub ahead of print.
Kaluza GL, Granada JF. The bioresorbable scaffold tale epilogue: overpromised, underdelivered, prematurely degraded. J Am Coll Cardiol Intv. 2019;Epub ahead of print.
Disclosures
- The VANISH trial was supported by Abbott Vascular and the Dutch Heart Foundation.
- Gori reports no conflicts of interest.
- Kaluza and Granada report institutional financial support from Abbott Vascular, Amaranth Medical, REVA Medical, Elixir Medical, and Meril Life Sciences.


Comments