Thrombectomy’s Benefits in Large-Core Strokes Sustained at 1 Year: TENSION
The procedure helps, but outcomes remain poor overall in this group. “We still have work to do,” Eva Mistry says.

BASEL, Switzerland—Among patients with large-core acute ischemic strokes, thrombectomy provides lasting benefits for up to 1 year compared with medical therapy alone, affirm new results from the TENSION trial.
At 12 months, patients who underwent the procedure had better functional outcomes and quality of life, with a lower rate of mortality or dependency, similar to what was seen in the main 90-day results, Götz Thomalla, MD (University Hospital Hamburg-Eppendorf, Germany), reported last week at the European Stroke Organisation Conference (ESOC) 2024.
Moreover, an improvement of at least 1 point on the modified Rankin Scale (mRS) between 90 days and 1 year was seen among those treated with thrombectomy (17%) as well as those who received medical therapy alone (11%).
The continuing advantage for thrombectomy in patients with large-core strokes over longer-term follow-up has now been seen in multiple trials, with TENSION joining SELECT2 and TESLA in providing 1-year results.
“The results are consistent,” Thomalla said. “There is a sustained long-term benefit of endovascular thrombectomy.”
Solidifying Evidence Around Large-Core Strokes
There have now been six randomized trials showing that patients with acute ischemic stroke caused by a large-vessel occlusion (LVO) that results in a large ischemic core—a group excluded from the initial spate of studies establishing thrombectomy as standard of care—derive a significant benefit from the intervention when compared with medical therapy alone. Those include RESCUE-Japan LIMIT, SELECT2, ANGEL-ASPECT, TENSION, TESLA, and LASTE. Data beyond 90 days, however, had been lacking until recently.
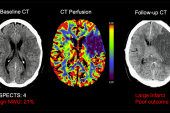
Here at ESOC, Thomalla reported 12-month results of the TENSION trial, which included 253 patients (median age about 73; 49% women) who had an LVO stroke and an ASPECTS of 3 to 5, indicating a large infarct, based on visual assessment of a noncontrast CT or MRI. For patients in the intervention group, thrombectomy using any available device was initiated within 12 hours of stroke onset or the time the patient was last known to be well. The median NIHSS score was 18 to19 at baseline, and 37% of patients received IV alteplase as part of medical treatment.
The primary outcome for this 12-month analysis, as for the main analysis, was functional status according to the mRS. At the later time point, the median mRS score was better in the thrombectomy arm than in the control arm (5 vs 6; P = 0.0004). The procedure also resulted in higher rates of mRS 0 to 2 (22% vs 6%; P = 0.004) and mRS 0 to 3 (34% vs 17%; P = 0.0035).
In addition, thrombectomy was associated with significantly better quality of life according to the EQ-5D instrument, health status according to the EQ visual analogue scale, and global physical health according to the PROMIS-10 measure (P < 0.05 for all). There were nonsignificant differences in anxiety and depression favoring thrombectomy.
The intervention also was associated with lower rates of mortality (58% vs 70%; HR 0.70; 95% CI 0.50-0.99) and mortality/dependency (66% vs 78%; OR 0.50; 95% CI 0.28-0.90) at 12 months, showing a maintained advantage for thrombectomy beyond 90 days.
Reassuring But Not Surprising
Commenting for TCTMD, Eva Mistry, MBBS (University of Cincinnati, OH), said these 1-year results are reassuring, if unsurprising. “We know that this is a powerful therapy. It has shown benefit in large-core strokes in [several] trials now.”
Two findings point to the need for further efforts to improve outcomes in this population, she said—the high level of disability that remained even after thrombectomy and the continuing gains in functional status among many patients after 90 days of follow-up.
“There is still a lot of work to do in the rehabilitation space to get the full benefit of that continued trajectory of improvement from 3 months onwards,” Mistry said. As for the overall poor outcomes, “I really hope that we’ll continue to take that as an indication that we need to make strides towards improving upon those outcomes even out to a year,” she added.
Typically, at least in the United States, poststroke rehabilitation—including physical, occupational, and speech therapy and other therapies—lasts about 3 months, with insurers often limiting the number of sessions that patients can attend, she noted.
“But I feel like we should definitely see this as an indication that we can work on improving outcomes out to longer than 3 months,” she said. “So not just the 20 sessions that are covered. Hopefully, there’ll be more space for research and then clinical care policymaking changes around those issues also.”
Working toward earlier stroke recognition and interventions that slow the progression to large ischemic cores may help improve outcomes overall, Mistry suggested, adding that she’s hopeful that research into neuroprotectants will eventually pay dividends as well.
“We still have work to do in these patients,” she said.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Thomalla G. Functional outcome and quality of life at 12 months after thrombectomy for stroke with extended lesion in the TENSION trial. Presented at: ESOC 2024. May 16, 2024. Basel, Switzerland.
Disclosures
- TENSION has received funding from the European Union’s Horizon 2020 research and innovation program. The academic sponsor was the University of Heidelberg.
- Thomalla reports receiving consulting or lecture fees from Acandis, Amarin, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol Myers Squibb/Pfizer, Daiichi Sankyo, and Stryker; receiving grants from the German Research Foundation, the European Union, the Corona Foundation, and the German Innovation Fund; serving as a member of the data and safety monitoring board for the TEA-Stroke trial; and serving a member of the ESO board of directors.




Comments