Tricuspid Repair During Mitral Surgery Slows Disease Progression at 2 Years
Practice to date has been mixed and while this trial adds data, the lack of a survival benefit means the impact on practice is unclear.

For patients with mild-to-moderate tricuspid regurgitation (TR) on top of degenerative mitral regurgitation (MR), tricuspid annuloplasty done at the time of mitral valve surgery can prevent disease progression but doesn’t impact the risk of death or other adverse outcomes at 2 years, data from a randomized controlled trial show.
Tricuspid repair did, however, increase the need for permanent pacemaker implantation by nearly sixfold, Cardiothoracic Surgical Trials Network (CTSN) researchers reported in a late-breaking session today at the virtual American Heart Association (AHA) 2021 Scientific Sessions. The results were published simultaneously in the New England Journal of Medicine.
James S. Gammie, MD (Johns Hopkins Heart and Vascular Institute, Baltimore, MD), speaking with the media, said that while there’s broad agreement that severe TR should be treated, “there is significant uncertainty about how to manage moderate-or-less tricuspid regurgitation.” Some observational data suggest that failure to address it impairs survival and increases the risk of heart failure, he said. Additionally, were the TR to become severe and require reoperation, the surgery carries high mortality.
Joanna Chikwe, MD (Cedars-Sinai Medical Center, Los Angeles, CA), who co-authored an editorial accompanying the paper’s publication, told TCTMD that many surgeons have been excitedly awaiting the new results. “For something that impacts a relatively focused group of patients, it’s been astonishing quite how much controversy, debate, and practice variation there has been around this exact question,” she said, pointing out that Gammie’s prior research has shown anywhere from 5% to 75% of patients across hospitals get concomitant tricuspid and mitral valve surgery.
“This trial has actually provided really helpful data. Certainly in the short term, it seems the appropriate strategy is to repair patients that have moderate tricuspid regurgitation if you expect them to have a good life expectancy,” Chikwe concluded.
Concern over the potential for injury is the chief reason why some surgeons are reluctant to treat less-than-severe TR, she said. Need for permanent pacemaker, the most pressing issue, can be reduced by optimizing surgical techniques, and the lengthier procedures with tricuspid annuloplasty, also a concern, haven’t translated into worse outcomes, said Chikwe.
No Difference in Death
At 39 centers in the United States, Canada, and Germany, CTSN investigators enrolled 401 patients with degenerative MR, randomizing them to receive tricuspid annuloplasty or no additional procedure on top of mitral valve surgery. All had either moderate TR, seen in 37% of the cohort, or none/trace or mild TR alongside tricuspid annular dilatation of 40 mm or more (or 21 mm/m2). Most (91%) were white, three-quarters were men, and their average age was 67 years.
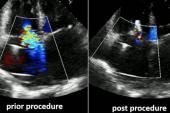
Approved, rigid, incomplete, nonplanar, and undersized (26, 28, or 30 mm) tricuspid annuloplasty rings were used for tricuspid valve repair, the NEJM paper notes. TR severity was measured by transthoracic echocardiography and verified by a central core lab.
Most procedural characteristics were similar in the two study arms, though cardiopulmonary bypass time was longer when tricuspid annuloplasty was added to mitral valve surgery (mean 166.1 vs 132.6 min).
The primary endpoint—a composite that included reoperation for TR, progression of TR by two grades from baseline or presence of severe TR, and death at 2 years—was reduced with the addition of tricuspid annuloplasty to mitral valve surgery (3.9% vs 10.2%; relative risk 0.37; 95% CI 0.16-0.86; P = 0.02). No reoperations occurred. Death rates were similar, however, in the two groups (3.2% vs 4.5%; RR 0.69; 95% CI 0.25-1.88). Instead, the difference was driven by progression of TR, which was less common in the surgery/annuloplasty group than among patients who only underwent mitral valve surgery (0.6% vs 6.1%; RR 0.09; 95% CI 0.01-0.69).
A post hoc analysis showed that patients with moderate TR at baseline—but not those with tricuspid annular dilatation and less-than-moderate TR—had a reduction in the primary endpoint (4.5% vs 18.1%; RR 0.25; 95% CI 0.07-0.83).
At 2 years, severe TR was seen in 0.6% of the annuloplasty/surgery group and in 5.6% of the surgery-alone group, while moderate/severe TR rates were 3.4% and 25.1%, respectively.
The addition of tricuspid annuloplasty had no effect on MACCE rate, functional status, or quality of life at 2 years, but did raise the risk of permanent pacemaker implantation over surgery alone (14.1% vs 2.5%; rate ratio 5.75; 95% CI 2.27-14.60).
“Long-term follow-up is ongoing to fully determine the net clinical benefit,” Gammie concluded.
Roxana Mehran, MD (Icahn School of Medicine at Mount Sinai, New York, NY), in discussion following Gammie’s presentation, said that there are lessons to be learned about the natural history of tricuspid valve disease.
“What I was struck by, I think, is that we as clinicians believe that if you fix the mitral valve, maybe the tricuspid regurgitation will improve. And it seems like that is not what’s happening,” she observed, adding, “Of course, it seems an annuloplasty should reduce TR progression. But certainly mitral valve surgery alone will not. And I think that is a huge takeaway.”
What Comes Next
Chikwe, in the media briefing, praised the CTSN effort for its large size. “I think this was a tremendous trial,” she said, pointing out the difficulty of powering randomized controlled trials for rare clinical outcome like death. One solution is to use an echocardiographic endpoint like regurgitation.
Progression to severe TR, though, is important in and of itself, Chikwe commented. “We know that eventually [severe TR] leads to liver failure, right heart failure, increased chances of death. For me, my take home from the trial was if I operated on 20 patients with moderate tricuspid regurgitation when I’m fixing the mitral valve, I could save one patient from having severe tricuspid regurgitation, maybe at the cost of two patients needing permanent pacemakers.
“For me, that trade-off is worth it,” she observed.
Chikwe’s editorial, written with co-author Mario Gaudino, MD (Weill Cornell Medicine, New York, NY), does provide some caveats. For example, the finding that severe TR wasn’t linked to worse clinical symptoms or quality of life “suggests that an aggressive approach to [annuloplasty] in high-risk patients with limited life expectancy is probably not warranted,” they write. “Similarly, the results challenge guideline recommendations to perform surgery in patients with lesser grades of tricuspid regurgitation, since almost none of these patients had progression to severe tricuspid regurgitation during short-term follow-up.
“The very dynamic nature of tricuspid regurgitation and wide variability in assessing tricuspid annular dilatation are additional compelling reasons to leave lesser regurgitation alone,” the editorialists continue, adding, “The most appropriate strategy for the treatment of milder tricuspid regurgitation may emerge from longer follow-up.”
For Gammie, whether their 2-year results will change practice remains to be seen. “There are some very fierce opinions in the cardiac surgery community around this issue. . . . I think a lot of folks will take away from this that moderate TR probably should be fixed, that putting that tricuspid annuloplasty [device] in arrests the progression of TR very, very effectively,” he said.
He pointed out that their data call into question US guidelines related to tricuspid annular dilatation, since progression in that subgroup was very rare with or without annuloplasty. Currently, the recommendations say tricuspid valve repair “can be beneficial” in patients with mild or moderate functional TR at the time of mitral valve surgery if there’s tricuspid annular dilatation (class II, level of evidence B).
Follow-up in their study is slated for at least 5 years, Gammie said. “And I think that with time we’ll see additional data that will be helpful.”
Chikwe agreed, emphasizing that “in cardiac surgery, it takes 3, 5, 10 years to really understand the net clinical benefit to patients.” Beyond forthcoming data from this trial, the “excitement will be around what transcatheter tricuspid valve repair can do in this space,” she noted to TCTMD.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Gammie JS, Chu MWA, Falk V, et al. Concomitant tricuspid repair in patients with degenerative mitral regurgitation. N Engl J Med. 2021;Epub ahead of print.
Chikwe J, Gaudino M. The price of freedom from tricuspid regurgitation. N Engl J Med. 2021;Epub ahead of print.
Disclosures
- The study was funded by the National Heart, Lung, and Blood Institute (NHLBI) and the German Center for Cardiovascular Research.
- Gammie reports being a consultant to and stockholder in Edwards Lifesciences.
- Chikwe reports being co-PI /study director of an NHLBI-sponsored CTSN trial of surgical versus transcatheter repair of primary MR (NCT05051033).
- Gaudino reports grants from the National Institutes of Health/NHLBI outside the submitted work.


Comments