Tricuspid Trio: TRISCEND, CLASP TR, and TriBAND Studies Show Advances
“We have to really push the boundaries to make the tricuspid options available, feasible, and safe,” says Thomas Modine.
Transcatheter therapies for tricuspid valve disease continue to gain momentum, as evidenced by three studies presented at this week’s EuroPCR 2021: TRISCEND, TriBAND, and CLASP TR.
On the whole, the early data suggest these devices are a viable treatment for tricuspid regurgitation (TR), investigators told the meeting’s virtual audience, yet they also speak to the diverse approaches—annular reduction, transcatheter edge-to-edge repair (TEER), and valve replacement—aimed at addressing this clinical niche.
All three are manufactured by Edwards Lifesciences:
- Thirty-day data from TRISCEND make the case for valve replacement, specifically with the Evoque device, in patients with symptomatic and at least moderate TR.
- From CLASP TR, there’s a 6-month report building on 30-day results released at last year’s TVT meeting; the latest findings continue to indicate that TEER with the Pascal device can, in experienced hands, be safely used in patients with symptomatic, severe TR.
- And finally, results from the TriBAND postmarketing study, which were simultaneously published online in EuroIntervention, confirm that the Cardioband system, an incomplete annuloplasty ring, can reduce TR in patients with symptomatic, severe disease at the time of hospital discharge, with favorable outcomes seen at 30 days.
Thomas Modine, MD, PhD (CHRU de Lille, France), commenting for TCTMD, said these therapies “are complementary actually, because it gives you more than one weapon to engage in this battle of treating the tricuspid regurg—and it is needed.”
Unlike percutaneous tricuspid interventions, which are technically challenging, surgery for TR is straightforward, said Modine. But because the condition often can be well managed for many years by diuretics, by the time patients “reach the point of no return” and need more-invasive treatment, they may be elderly or at high risk for surgery.
“We have to push the field, we have to develop new therapies, we have to really push the boundaries to make the tricuspid options available, feasible, and safe,” Modine urged. All three of the aforementioned devices were originally designed to treat the mitral valve before being brought to the tricuspid setting. “None of these available today were initially thought or imagined to treat the tricuspid,” he pointed out, so subsequent iterations should be tailored to tricuspid anatomy.
Results from the multicenter TriValve Registry, also presented at EuroPCR, offer insight into what factors determine a good response to the breadth of tricuspid options—from various companies using different strategies—that are being applied in real-world practice.
TRISCEND
EuroPCR featured one late-breaking presentation on transcatheter tricuspid valve replacement: the TRISCEND study of the Evoque device.
For TRISCEND, “a young study with a new treatment, the results are very interesting so far,” said Modine, adding this approach is a logical next step after TEER, “because replacement is technically much easier.”
During EuroPCR and at least week’s American College of Cardiology 2021 Scientific Session, Susheel Kodali, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), shared the latest data from TRISCEND. Evoque notably is “designed to be delivered from a transfemoral approach over a stiff wire placed in the RV apex,” Kodali said, adding, “The self-expanding nitinol valve engages the leaflets, chords, and annulus to achieve secure placement.”
TRISCEND enrolled 56 patients, 84% of whom were NYHA functional class III-IV; 92% had at least severe TR. For 68%, the etiology of TR was functional, whereas 11% had degenerative TR and the rest had mixed/other origins. Nine in 10 had atrial fibrillation. Nearly half (43%) had undergone a prior valve surgery or intervention.
Baseline TR grade was severe in 46%, massive in 29%, and torrential in 15%. By 30-day follow-up, however, 98% had mild or none/trace TR. All patients had a reduction of at least one TR grade and 95% had a decrease of two or more grades. Three-quarters were NYHA class I-II. There were significant improvements in 6-minute walk distance and Kansas City Cardiomyopathy Questionnaire (KCCQ) score.
At 30-day follow-up, one patient (1.9%) had died of a cardiovascular cause. There were no strokes or MIs. Severe bleeding, the most-common complication, was seen in 12 patients (22.6%), while two (3.8%) required nonelective tricuspid valve reintervention and one (1.9%) had major access-site/vascular complications. Two patients died in total, for an all-cause mortality rate of 3.8%
“Based on the results of this study, a pivotal trial evaluating this therapy”—TRISCEND II—"has been initiated,” Kodali concluded.
Despite Modine’s interest in Evoque, he did mention a counterpoint. Replacement leaves “a lot of material in the heart, so this can lead to thrombosis,” he observed, noting that this requires patients to be put on anticoagulation at the risk of increased bleeding. Indeed, among the three studies presented at EuroPCR, bleeding was most common in TRISCEND, Modine pointed out.
Additionally, any bioprosthesis has the potential to degenerate. “It has a limited time [of] durability, and in that case you have to be sure that you can come and put a new valve in it. This is why we avoid transcatheter tricuspid valve replacement, although it’s a very effective therapy. And this is where we have to wait for more studies, more patients, younger ones, with longer expectancy of life, to see where we can put the ‘cursor.’”
CLASP TR
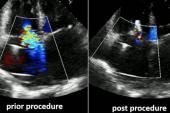
Mackram Eleid, MD (Mayo Clinic, Rochester, MN), presenting the latest results from CLASP TR for TEER with the Pascal device, showed that much like at 30 days, 6-month results in these challenging cases of tricuspid valve disease are encouraging. (Also at EuroPCR, as reported by TCTMD, 2-year data from the single-arm CLASP study in mitral valve disease showed the Pascal device can offer high rates of survival and freedom from rehospitalization, as well as a durable reduction in mitral regurgitation.)
Seventy percent of the 63 patients had started out with NYHA class III-IV at baseline. Six months later, 84% were NYHA class I-II. At baseline, TR was categorized in 69% as “massive or torrential,” a proportion that dropped to 8% by 6 months. Within 6 months, 89% improved by at least one TR grade and 70% saw at least a two-grade reduction in TR. There were significant gains in quality life on the KCCQ.
At 6-month follow-up, two patients each (2.3%) had died of CV causes or experienced stroke, and there were no MIs. Severe bleeding occurred in five patients (7.9%), while reintervention related to the device and major access-site/vascular complications requiring intervention were seen in one patient (1.6%) each. Other events included all-cause death (3.2%), heart failure hospitalization (6.3%), and single-leaflet device attachment assessed by a core lab (4.8%).
Pascal, which received CE Mark approval last year in Europe, “has emerged as a viable option for treating patients with severe TR,” Eleid concluded. In the United States, the CLASP II TR pivotal trial is underway.
Modine, though he praised Pascal for being less complex than annuloplasty-based transcatheter repair, said there is a downside: “This is an incomplete solution, because usually the disease makes the gap very large in the tricuspid setting and usually you cannot eliminate your regurg, you just reduce it.” Even if the TR improves from severe to moderate, for instance, “because the primary disease is still there, it can keep on evolving and you have a recurrence,” he observed.
TriBAND
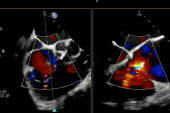
Cardioband, which repairs the annulus, also is progressing down the pike.
Georg Nickenig, MD (University Hospital Bonn, Germany), presenting the TriBAND data, reminded EuroPCR attendees that the Cardioband device is designed to reduce annular dilation, allowing better leaflet coaptation, “which is the key pathology of functional tricuspid regurgitation.” A series of anchors help anchor the device in the tricuspid annulus which is then cinched smaller. He noted that Cardioband—originally developed for mitral regurgitation—was the first device, in 2018, to receive CE Mark approval for the tricuspid indication.
The TriBAND study included 61 patients with severe and symptomatic functional TR who hadn’t responded to diuretic therapy. Most (85%) were NYHA class III-IV at baseline. By discharge, 59% had reached moderate-or-lower-grade TR, with 78% showing a reduction of at least one grade. Septolateral annular diameter decreased by 20%, the researchers note in EuroIntervention, pointing out that these changes were “accompanied by early evidence of right heart remodeling.”
At 30-day follow-up, there was one MI (1.6%) but no CV mortality or stroke. There was one all-cause death. The most common complications were severe bleeding, in seven patients (11.5%); major access-site/vascular complications and coronary artery injury requiring intervention, each seen in four patients (6.6%); and new need for renal replacement therapy, in two patients (3.3%). The majority (74%) were now in NYHA class I-II, and overall KCCQ score had improved by 17 points.
Nickenig et al conclude that Cardioband “uniquely addresses a fundamental pathology of functional TR, ie, dilatation of the tricuspid annulus. By addressing the annulus and maintaining the native tricuspid leaflets, the Cardioband tricuspid system preserves the option for future interventions such as leaflet repair or valve replacement.”
To TCTMD, Modine pointed out that among the three approaches, Cardioband most closely mimics surgical approaches to TR. But “band implantation is not always easy, because it depends hugely on the quality of imaging, and imaging today even with the best echocardiographers is still very limited because you have interferences between the device that you put in the patient and the echo imaging. And [sometimes] it doesn’t render enough quality in order to see correctly,” he explained.
TriValve Registry
There’s the question, though, of how all these technologies are playing out in real-world use. Presenting data from the TriValve Registry, Mara Gavazzoni, MD (University Hospital Zurich, Switzerland), said it “represents the largest worldwide series of patients treated with transcatheter tricuspid interventions in routine clinical practice [outside of] trials.”
TriValve is tracking procedures that involve repair of the leaflets with MitraClip (Abbott) or Pascal; the annulus with Cardioband, TriCinch (4tech), or TriAlign (Mitralign); and the coaptation with Forma (Edwards Lifesciences), as well as tricuspid valve replacement with NaviGate (NaviGate Cardiac Structures).
As a whole, she said, transcatheter treatments provide a 1-year freedom from death/rehospitalization rate exceeding 75%. But what of the patients who neither die nor return to the hospital for heart failure (HF)?
Median follow-up duration was 6 months. Among 453 patients in TriValve with information available on dyspnea/NYHA class, peripheral edema, and ascites, 43% were classified as good responders (improvement of at least 50% in their baseline risk factors), 42% as intermediate responders (gains of less than 50% or at least one risk factor worsened, without HF hospitalization), and 15% as nonresponders (hospitalization for HF).
Ascites at baseline independently predicted an 80% lower likelihood of good response and a 50% lower likelihood of intermediate response. Acute procedural success resulting in TR grade ≤ 2+ tripled the odds of good response and doubled the odds of response. Persistence of TR grade ≤ 2+ over time, too, was tied to response.
Among responders, “a relatively greater symptomatic effect is observed in those patients [with] more-disabling baseline symptoms and more LV advanced disease,” Gavazzoni reported.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Nickenig G, Friedrichs K, Baldus S, et al. Thirty-day outcomes of the Cardioband tricuspid system for patients with symptomatic functional tricuspid regurgitation: the TriBAND study. EuroIntervention. 2021;Epub ahead of print.
Eleid M. Transcatheter valve repair in patients with severe tricuspid regurgitation: six-month results of the CLASP TR early feasibility study. Presented at: EuroPCR 2021.
Kodali S. Transfemoral tricuspid valve replacement: TRISCEND study 30-day results. Presented at: EuroPCR 2021.
Gavazzoni M. Clinical Response to Transcatheter treatment of tricuspid regurgitation. Presented at: EuroPCR 2021.
Disclosures
- Kodali reports serving as a consultant to Admedus (now Anteris Technologies) and Dura Biotech; having equity in Thubrikar Aortic Valve, Dura Biotech, Supria, Microinterventional Devices, Admedus, and Triflo; and receiving institutional funding from Edwards Lifesciences, Medtronic, Boston Scientific, Abbott Vascular, and JenaValve.
- Eleid reports no relevant conflicts of interest.
- Nickenig reports receiving speakers honoraria or travel/grant support from Edwards Lifesciences. He also has received research funding from the Deutsche Forschungsgemeinschaft (DFG), the Federal Ministry of Education and Research (BMBF), the European Union, Abbott, AGA Medical, AstraZeneca, Bayer, Berlin Chemie, BioSensus, Biotronik, Bristol-Myers Squibb, Boehringer Ingelheim, Daiichi Sankyo, Edwards Lifesciences, Medtronic, Novartis, Pfizer, Sanofi, and St. Jude Medical; has received honoraria for lectures or advisory boards from Abbott, AGA Medical, AstraZeneca, Bayer, Berlin, Cardiovalve, Berlin Chemie, BioSensus, Biotronik, Bristol-Myers Squibb, Boehringer Ingelheim, Daiichi Sankyo, Medtronic, Novartis, Pfizer, Sanofi, and St. Jude Medical; and has participated in clinical trials for Abbott, AGA Medical, AstraZeneca, Bayer, Berlin Chemie, BioSensus, Biotronik, Bristol-Myers Squibb, Boehringer Ingelheim, Cardiovalve, Daiichi Sankyo, Edwards Lifesciences, Medtronic, Novartis, Pfizer, Sanofi, and St. Jude Medical.
- Gavazzoni reports being a consultant to Abbott Vascular.
- Modine reports serving as a consultant to Abbott, Edwards Lifesciences, and Medtronic.



Comments